Research Article
Assessing the Impact of Ginger and Clove on Postoperative Pain Following Inguinal Hernia and Testicular Varicocele Surgeries
- Mohammad Alipour
- Atefeh Shahroudi *
- Sara Khashkhashi Moghadam
Department of Anesthesiology, Ghaem Hospital, Mashhad University of Medical Sciences, Mashhad, Iran.
*Corresponding Author: Atefeh Shahroudi, Department of Anesthesiology, Ghaem Hospital, Mashhad University of Medical Sciences, Mashhad, Iran.
Citation: Alipour M., Shahroudi A., Moghadam S. K. (2024). Assessing the Impact of Ginger and Clove on Postoperative Pain Following Inguinal Hernia and Testicular Varicocele Surgeries, International Journal of Biomedical and Clinical Research, BioRes Scientia Publishers. 1(6):1-8. DOI: 10.59657/2997-6103.brs.24.033
Copyright: © 2024 Atefeh Shahroudi, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: September 30, 2024 | Accepted: November 25, 2024 | Published: December 02, 2024
Abstract
Introduction: Postoperative pain is often moderate to severe and peaks within the first 24 h. Drugs, such as NSAIDs or opioids, are commonly used to manage pain. In this context, the effects of herbal medicines, such as ginger and clove, have not been extensively studied. This study aimed to investigate the effects of ginger and clove on pain following inguinal hernia and testicular varicocele surgery.
Material and Methods: This clinical trial included 92 patients who were candidates for inguinal hernia or testicular varicocele surgery at the Ghaem Hospital, Mashhad University of Medical Sciences, Mashhad, Iran, between 2022 and 2023. All patients were ASA class I or II and were divided into four groups: clove (first group), ginger (second group), clove + ginger (third group), and control (fourth group). Pain scores, amount of diclofenac suppositories and narcotics used, and nausea, vomiting, and chills were evaluated in recovery time, 2, 4, 6, 12, and 24 h post-surgery. All analyses were performed using SPSS software, and a P-value of less than 0.05 was considered statistically significant.
Result: Each group comprised of 24 patients. The mean ages were 48.22±10.40, 41.65±14.11, 41.64±12.65, and 37.54±7.52 in the ginger, clove, ginger and clove, and control groups, respectively. The NSAID dose used in the control group was significantly higher than that in the other groups during recovery and at 1, 12, and 24 h after surgery (P<0.05). Pain scores during recovery were significantly higher in the control group than in the other groups (P<0.05). At 2, 4, 6, 12, and 24 h post-surgery, pain scores were significantly higher in the ginger group and lowest in the control group than in the other groups (P<0.05). There were no significant differences in postoperative complications, anesthesia time, or ASA between the groups (P>0.05).
Conclusion: The combination of cloves and ginger as analgesic agents can serve as a non-narcotic treatment option for managing mild-to-moderate postoperative pain. Further studies and evaluations are needed to determine the appropriate and effective doses of clove and ginger for pain reduction.
Keywords: clove; ginger; postoperative pain
Introduction
Postoperative pain can often be attributed to tissue manipulation during the procedure. This manipulation can lead to several types of pain, including pain at the site of the surgical incision due to tissue damage (incisional pain); pain from the manipulation of muscles, ligaments, and other deep tissues (deep tissue pain); pain resulting from the body’s inflammatory response to surgery (inflammatory pain); and pain caused by nerve damage or irritation during surgery (neuropathic pain) [1]. Postoperative pain resulting from the manipulation of tissues by the surgeon is often moderate to severe, peaking within the first 24 hours. Medications such as non-steroidal anti-inflammatory drugs (NSAIDs) and opioids can be used to effectively manage pain [2]. However, both NSAIDs and opioids have side effects. NSAIDs can cause stomach ulcers, bleeding, and gastritis owing to their effects on the stomach lining [3]. They can also impair kidney function, especially in patients with preexisting kidney conditions. The long-term use of NSAIDs can increase the risk of heart attack and stroke [4]. On the other hand, opioids can cause nausea and vomiting, respiratory depression, constipation, and carry a risk of dependence and addiction [5].
Herbal remedies play a significant role in pain management after surgery. Credible medical literature provides extensive information on alternative methods for postoperative pain management [6]. The analgesic and opioid-like activities of various herbs traditionally used for pain relief may explain their effectiveness. Combining the right herbs can produce beneficial synergistic effects [6]. For example, ginger (Zingiber officinale) [7], turmeric (Curcuma longa) [8], clove (Syzygium aromaticum) [9], willow bark (Salix spp.), and etc., enhance the analgesic effects of medications such as ibuprofen or morphine.
Ginger, also known as Zingiber officinale, is a plant root that has been used in traditional medicine for centuries. It contains many compounds, including gingerol, pinene, cineole, capsaicin, beta-carotene, caffeic acid, and curcumin [10]. Gingerol can be converted to 6-paradol and 6-shogaol, both of which have antipyretic (anti-fever) and anti-inflammatory effects. Ginger is absorbed after oral dosing and has an elimination half-life of less than 2 hours [11]. Oyedemi et al. indicated that gingerols function as agonists of vanilloid receptors, suggesting that ginger may alleviate inflammatory pain [12]. Current evidence from in vitro and animal model studies has demonstrated that various compounds in ginger possess antioxidative and anti-inflammatory activities. These properties may be effective in reducing symptoms of chronic inflammatory diseases, particularly pain [13]. Ginger complications have been observed in patients with gallstones, kidney stones, and coagulation problems. However, in healthy individuals administered therapeutic doses, there were no specific complications [14].
Clove, a plant from the Myrtaceae family known as Syzygium aromaticum, has been used for centuries in traditional medicine as a local anesthetic to treat toothaches, headaches, and joint pain. This plant contains phenolic compounds, such as flavonoids, hydroxybenzoic acid, hydroxycinnamic acid, and hydroxyphenylpropene [15]. Clove exhibits antioxidant, analgesic, anti-spasmodic, and antimicrobial effects. Its analgesic properties are primarily due to eugenol, which activates calcium and chloride channels in the trigeminal ganglion receptors, and the presence of capsaicin agonists [16]. The side effects of clove at doses higher than 150 mg/kg per day include severe skin irritation, liver failure, and severe gastrointestinal problems, which have not been approved by the World Health Organization (WHO)-approved dose [17].
The analgesic effects of ginger and clove have been previously demonstrated. However, few clinical trials have been conducted to determine whether these herbs are suitable replacements for routine treatment. Therefore, this study aimed to investigate the effects of ginger and clove on pain following inguinal hernia and testicular varicocele surgeries.
Materials and Methods
Study Population
This clinical trial included 92 patients who were candidates for inguinal hernia or testicular varicocele surgery at the Ghaem Hospital, Mashhad University of Medical Sciences, Mashhad, Iran, between 2022 and 2023. Men aged 16 to 60 years who underwent inguinal hernia or testicular varicocele surgery and were classified as ASA class I or II were included in the study. Conversely, patients with autoimmune disorders, addictions, contraindications for the study drugs, gastrointestinal diseases, cardiovascular diseases, hepatic disease, renal disease, convulsive disease, and diabetes problems were excluded from the study.
In this double-blind study, sealed opaque envelopes were used to conceal sequencing. Both the participants and the person responsible for data collection were blinded to group allocation and treatment type. The patients were randomly assigned to four groups using random blocks. The groups were as follows: clove (first group), ginger (second group), clove + ginger (third group), and control (fourth group).
Study Protocol
Based on the half-life of ginger and clove oil (eugenol) and previous studies [17,18], the dosages used were 2.5 mg/kg of ginger (Kharazmi Pharmaceutical Company, Iran) and 3 mg/kg of clove oil (Adonis Gol Darou Company, Iran). Accordingly, the first group received 2.5 mg/kg of ginger, the second group received 3 mg/kg of clove oil, the third group received both 3 mg/kg of clove oil and 2.5 mg/kg of ginger, and the fourth group, serving as the control group, received a placebo (identical in color and shape, made by Mashhad Medical Sciences Faculty). The treatments were administered orally 90 min before and 2 h after the surgery. Finally, each patient’s pain was assessed using a visual analog scale (VAS; 0, no pain; 5, moderate pain; and 10, worst possible pain). The use of diclofenac suppositories (maximum 2 doses of 100 mg each), narcotics, nausea, vomiting, and chills was evaluated before surgery, and at 2, 4, 6, 12, and 24 h after surgery. If the pain score was between 7 and 10, then pethidine was administered.
Statistical Analysis
Analysis of variance (descriptive data are summarized as means, standard deviations, and/or percentages) and the normality of the data were checked prior to analysis using the One-Sample Kolmogorov-Smirnov test. ANOVA or its non-parametric equivalent was used for quantitative variables, and Burley’s repeat was applied. All analyses were performed using the SPSS software (version 25, Chicago, IL, USA). Statistical significance was set at p lessthan 0.05.
Ethical Considerations
The Ethics Committee of Mashhad University of Medical Sciences reviewed and approved the study protocol as part of its review and approval of the research project (No: IR.MUMS.REC.1396.193).
Results
This study included 92 patients who were eligible for inguinal hernia or testicular varicocele surgery. Each group consisted of 24 patients. The mean ages were 48.22±10.40, 41.65±14.11, 41.64±12.65, and 37.54±7.52 in the ginger, clove, ginger and clove, and control groups, respectively. Statistical analysis revealed significant differences in age among the four groups (P=0.019). The control group had the lowest mean age, whereas the ginger group had the highest. The clove group and the ginger and clove group had similar mean ages. Additionally, the mean anesthesia times were 88.26±32.70, 73.7±11.89, 88.86±18.89, and 86.88±24.22 minutes in the ginger, clove, ginger and clove, and control groups, respectively. There were no significant differences in the duration of anesthesia between the four groups (P=0.094). The frequencies of the ASA classification and type of surgery are shown in Table 1. The frequency of surgery was significantly different between the groups (p lessthan 0.001). However, the anesthesia time and ASA classification showed no significant differences between the groups (p greaterthan 0.05).
Table 1: Frequency of ASA classification and types of surgery.
| Variables | Group | P-value | ||||
| Ginger | Clove | Ginger and Clove | Control | |||
| ASA-N (%) | I | 20 (87.0) | 17 (73.9) | 19 (86.4) | 21 (87.5) | 0.540 |
| II | 3 (13.0) | 6 (26.1) | 3 (13.6) | 3 (12.5) | ||
| Type of Surgery-N (%) | Inguinal Hernia Unilateral | 18 (78.3) | 12 (52.2) | 21 (95.5) | 11 (45.8) | 0.001 |
| Varicocele | 0 (0.0) | 11 (47.8) | 1 (4.5) | 0 (0.0) | ||
| Both | 0 (0.0) | 0 (0.0) | 0 (0.0) | 13 (54.2) | ||
| Inguinal Hernia Bilateral | 5 (21.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
The postoperative complication frequency showed that vomiting was not observed in patients at any of the time points considered. One patient (4.5%) in the ginger and clove groups experienced nausea during the recovery. Additionally, one patient (4.5%) in the ginger and clove groups and three patients (13%) in the ginger group exhibited symptoms of shivering during recovery. However, no nausea, shivering, or vomiting events were observed at 2, 4, 6, 12, or 24 h after surgery. Nausea and shivering showed no significant differences between groups during recovery (p>0.05) (Table 2).
Table 2: Frequency of complication in recovery time.
| Variables | Group | P-value | ||||
| Ginger | Clove | Ginger and clove | Control | |||
| Nausea N (%) | Yes | 0 (0.0) | 0 (0.0) | 1 (4.5) | 0 (0.0) | 0.359 |
| No | 23 (100) | 23 (100) | 21 (95.5) | 24 (100) | ||
| Shivering N (%) | Yes | 3 (13.0) | 0 (0.0) | 1 (4.5) | 0 (0.0) | 0.097 |
| No | 20 (87.0) | 23 (100) | 21 (95.5) | 24 (100) | ||
The doses of NSAIDs and pethidine administered after surgery are shown in Table 3. Statistical analysis revealed that the number of NSAIDs used post-surgery was significantly different between the groups during recovery (p=0.000), and at 2 h (p=0.001), 4 h (p=0.013), and 6 h (p=0.016) after surgery. Furthermore, the dose of pethidine was significantly different between the groups during recovery (p=0.020) and at 2 h (p=0.021) post-surgery. The highest and lowest doses were observed in the control and clove groups, respectively.
Table 3: Frequency of analgesics after surgery.
| Variables | Group | P-value | |||||
| Ginger | Clove | Ginger and Clove | Control | ||||
| NSAIDs-N (%) | Recovery | 0 | 23 (100) | 23 (100) | 22 (100) | 24 (100) | 0.000 |
| 1 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| 2 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 12 (50) | |||
| 1h After Surgery | 0 | 21 (91.3) | 20 (87.0) | 21 (95.5) | 19 (79.1) | 0.214 | |
| 1 | 0 (0.0) | 0 (0.0) | 1 (4.5) | 0 (0.0) | |||
| 2 | 2 (8.7) | 3 (13.0) | 0 (0.0) | 5 (0.20) | |||
| 2h After Surgery | 0 | 20 (87.0) | 23 (100) | 21 (95.5) | 18 (75) | 0.001 | |
| 1 | 3 (13.0) | 0 (0.0) | 1 (4.5) | 0 (0.0) | |||
| 2 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 6 (25) | |||
| 4h After Surgery | 0 | 20 (87.0) | 16 (69.6) | 22 (100) | 22 (92) | 0.013 | |
| 1 | 3 (13.0) | 2 (8.6) | 0 (0.0) | 0 (0.0) | |||
| 2 | 0 (0.0) | 5 (21.8%) | 0 (0.0) | 2 (8.0) | |||
| 6h After Surgery | 0 | 20 (87.0) | 23 (100) | 20 (90.9) | 24 (100) | 0.016 | |
| 1 | 3 (13.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| 2 | 0 (0.0) | 0 (0.0) | 2 (9.1) | 0 (0.0) | |||
| 1 h After Surgery | 0 | 23 (100) | 23 (100) | 21 (95.5) | 21 (87) | 0.092 | |
| 1 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| 2 | 0 (0.0) | 0 (0.0) | 1 (4.5) | 3 (13) | |||
| 24h After Surgery | 0 | 23 (100) | 23 (100) | 22 (100) | 23 (95) | 0.413 | |
| 1 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (5) | |||
| 2 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| Pethidine (mg) (Mean±SD) | Recovery | 4.35±6.62 | 0.00 | 4.09±7.96 | 6.67±9.63 | 0.020 | |
| 1h After Surgery | 2.61±6.89 | 1.74±5.76 | 3.18±7.16 | 7.50±7.90 | 0.028 | ||
| 2h After Surgery | 0.00 | 0.00 | 0.45±2.13 | 0.00 | 0.364 | ||
| 4h After Surgery | 1.74±5.76 | 0.00 | 0.91±4.26 | 0.00 | 0.286 | ||
| 6h After Surgery | 0.00 | 0.00 | 1.09±4.26 | 0.00 | 0.067 | ||
| 12h After Surgery | 0.00 | 0.00 | 0.00 | 0.00 | 1.000 | ||
| 24h After Surgery | 0.26±0.69 | 0.00 | 0.09±0.43 | 0.00 | 0.100 | ||
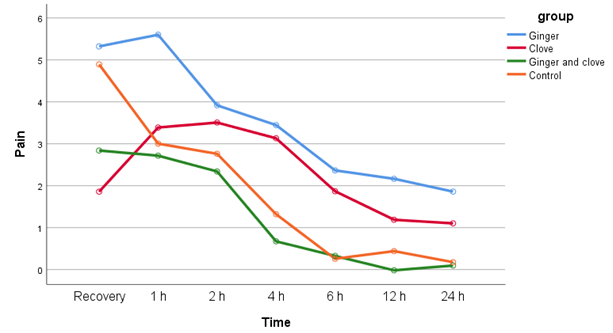
The mean pain scores at the different time points are shown in Table 4. The results showed that the pain scores at all times were significantly different between the groups (p lessthan 0.001). The highest and lowest pain scores during recovery were observed in the control and clove groups, respectively. One-hour post-surgery, the highest and lowest scores were observed in the ginger and clove groups, respectively. At 2, 4, 6, 12, and 24 h post-surgery, the highest scores were observed in the ginger group, while the lowest scores were observed in the control group.
Table 4: The pain scores after surgery based on group.
| Time [Mean±SD (95% CI)] | Group | P-value | |||
| Ginger | Clove | Ginger and Clove | Control | ||
| Recovery | 4.83±1.75 (4.07-5.58) | 1.57±1.12 (1.08- 2.05) | 3.36±1.53 (2.69- 4.04) | 5.17±1.37 (4.59-5.75) | <0> |
| 1h After Surgery | 5.17±2.01 (4.30-6.05) | 2.96±2.90 (1.70–4.21) | 4.77±1.90 (3.93 – 5.62) | 3.04±0.81 (2.70 – 3.38) | <0> |
| 2h After Surgery | 4.00±1.88 (3.19-4.81) | 3.13±1.36 (2.54-3.72) | 3.68±1.73 (2.92- 4.45) | 2.50±0.78 (2.17- 2.83) | 0.002 |
| 4h After Surgery | 3.35±1.97 (2.50-4.20) | 2.74±.96 (2.32- 3.16) | 2.27±1.86 (1.45- 3.10) | 1.04±.81 (.70- 1.38) | <0> |
| 6h After Surgery | 2.48±1.93 (1.64-3.31) | 1.57±1.12 (1.08-2.05) | 1.59±1.92 (.74 – 2.44) | 0.00 | <0> |
| 12h After Surgery | 2.09±1.81 (1.31-2.87) | 0.96±1.11 (.48–1.44) | 0.73±1.35 (.13- 1.33) | 0.17±0.38 (.01 - .33) | <0> |
| 24h After Surgery | 1.22±1.86 (.41- 2.02) | 0.96±1.11 (.48- 1.44) | 0.73±1.35 (.13 – 1.33) | 0.00 | 0.003 |
The effect of the interventions on pain scores over time, adjusted for age, pethidine dosage, and NSAID dosage, was significantly different between the groups (F=5.070; p=0.003). Moreover, we found similar results for the interaction between group and surgery type (F=8.328; p=0.005).
Table 5: Changes in pain scores over time based on groups.
| Variables | Type III Sum of Squares | df | Mean Square | F | P-Value | Partial Eta Squared |
| Age | 2.325 | 1 | 2.325 | 0.602 | 0.440 | 0.007 |
| Total Pethidine | 265.045 | 1 | 265.045 | 68.656 | 0.000 | 0.459 |
| Total NSAID | 23.407 | 1 | 23.407 | 6.063 | 0.016 | 0.070 |
| Group | 58.723 | 3 | 19.574 | 5.070 | 0.003 | 0.158 |
| Type of Surgery | 77.577 | 3 | 25.859 | 6.698 | 0.000 | 0.199 |
| Group and Type of Surgery | 32.150 | 1 | 32.150 | 8.328 | 0.005 | 0.093 |
The changes in pain scores over the duration of the study, adjusted for age, pethidine dosage, and NSAID dosage, for the four groups are shown in Figure 1.
Figure 1: Comparing the effects of ginger, ginger and clove, clove on pain after surgery with control during the time (Covariates appearing in the model are evaluated at the following values: Age, Pethidine dosage, and NSAID dosage).
Discussion
The main finding of the current study was that in terms of age, the ginger group had the highest mean age, while the control group had the lowest mean age. The dose of NSAIDs used in the control group was significantly higher than that in the other groups during the recovery time and at 1, 12, and 24 h after surgery. Furthermore, during the recovery time and at 2 hours after surgery, the dose of pethidine used was significantly lower in the clove group and highest in the control group compared to the other groups. Pain scores during recovery were significantly higher in the control group than in the other groups. At 2, 4, 6, 12, and 24 h post-surgery, pain scores were significantly higher in the ginger group and lowest in the control group than in the other groups. There were no significant differences in the postoperative complications between the groups.
Postoperative pain after inguinal hernia and testicular varicocele surgery, defined as groin pain lasting beyond three months, affects 30%-40% of patients, with severe cases in 1%-3%. The causes are not well understood, making it difficult to predict who will develop it. Therefore, it is crucial to use appropriate treatments to prevent postoperative pain [19].
The use of clove as a natural analgesic has attracted considerable interest owing to its potent pain-relieving and anti-inflammatory properties. Clove essential oil has traditionally been used in aromatherapy to relieve headaches, joint pain, and toothaches, as well as serving as an oral antiseptic [9]. Clove, particularly its active compound, eugenol, has been traditionally employed in various cultures for pain and inflammation management [20]. Eugenol, the primary bioactive component of clove, exhibits significant analgesic and anti-inflammatory effects. Research has indicated that eugenol can inhibit cyclooxygenase (COX) enzymes, which are crucial in the inflammatory process. This inhibition helps mitigate inflammation and pain; therefore, clove is a promising candidate for post-surgical pain management [21]. Clinical studies support the efficacy of cloves in relieving pain. For example, one study found that clove oil effectively reduced pain during intraoral injections in children, which was comparable to the pain relief provided by ice [22]. Esmaeili et al. reported that clove has been used in dental emergencies as an effective reliever for toothache and as an anti-inflammatory agent for the mouth and throat [23]. Additionally, Havale et al. demonstrated that clove oil was more effective than lignocaine gel, a commonly used local anesthetic. These findings suggest that clove could serve as a valuable adjunct to conventional postoperative pain management strategies [24]. Rahul Chandran et al. found in their in vivo study that a higher dose (200 mg/kg) of the extract was effective in reducing pain and inflammation [25]. In the current study, we used an aqueous solution of cloves at a dose of 2.5 mg/kg, based on the safe dose established by the WHO, which developed an Acceptable Dietary Intake (ADI) value of 2.5 mg/kg per day. The results of the current study showed that the dose of pethidine used was significantly lower in the clove group than in the other groups. Additionally, pain scores were significantly lower in the clove group than in the control group during the recovery period.
Ginger is well-known for its medicinal properties, especially in pain management and anti-inflammatory contexts. The bioactive compounds present in ginger, including gingerols and shogaols, have been extensively studied for their ability to alleviate pain and reduce inflammation. These properties suggest that ginger is a promising option for postsurgical pain relief [26]. Ginger is used for its anti-inflammatory, antioxidant, antiemetic, and pain-reducing effects, and can modulate pain through various mechanisms [27]. It contains 80-90 non-volatile compounds that contribute to its anti-inflammatory, antioxidant, and antiemetic properties. Ginger also reduces pain by inhibiting prostaglandins via the COX and LOX pathways, exhibiting antioxidant activity, inhibiting the transcription factor NF-κB, and acting as an agonist of vanilloid nociceptors [14]. Martins et al. reported that ginger significantly decreased migraine headaches and symptom severity compared to sumatriptan [28]. Kashefi et al. [29] and Rahnama et al. [30] found that ginger significantly alleviated primary dysmenorrhea in patients treated with ginger for five days, starting two days before the onset of menstruation. Another study demonstrated that ginger extract was effective in reducing pain and improving functional outcomes in patients with osteoarthritis, suggesting its potential benefits in the postoperative setting [31]. Our study showed that the dose of pethidine consumed in the ginger group was significantly lower than that in the control group but higher than that in the clove group. Additionally, ginger significantly reduced pain during recovery compared with in that the control group. However, at 2, 4, 6, 12, and 24 hours after surgery, the pain scores in the ginger group were significantly higher than those in the other groups. This may be due to age differences among the groups, as the control group had a significantly younger age profile. Furthermore, during recovery, the dosage of NSAIDs and pethidine was higher in the control group, which may have influenced the pain results in subsequent hours.
Age can significantly influence pain perception and management, particularly in postoperative settings. Older adults may experience changes in pain perception owing to physiological alterations in the nervous system, which can result in either heightened sensitivity to pain (hyperalgesia) or reduced sensitivity (hypoalgesia) [32]. Additionally, older adults often have slower metabolism, which affects the process of drug processing in the body. This necessitates careful dosing and monitoring to avoid side effects and inadequate pain relief. Furthermore, age can affect the speed of recovery and healing after surgery, with older adults typically experiencing a slower healing process. This can prolong the duration of pain and highlight the need for effective pain management strategies [33]. In our study, the control group had the lowest age range, whereas the ginger group had the highest age range. The clove and combined clove and ginger groups were similar in terms of age. Although, the control group exhibited higher pain levels during the recovery phase than the other groups, while the older ginger group experienced greater pain than the other groups. Conversely, the control group, with the youngest age range, reported less pain than did the other groups.
In general, the results from the present study showed that ginger and cloves significantly relieved pain in patients during the recovery phase compared with the control group, with the greatest pain relief observed in the combined ginger and clove groups. Additionally, there were no significant differences in postoperative complications between the groups. Although ginger and cloves have shown promising benefits, it is important to consider potential side effects and interactions. High doses of ginger and cloves can cause gastrointestinal (GI) upset in some individuals.
Owing to their analgesic and anti-inflammatory properties, ginger and cloves are valuable options for post-surgical pain management. The results of the present study showed that the use of ginger and cloves decreased the need for NSAIDs and pethidine. Using these natural remedies as adjunctive therapies alongside conventional pain relievers can enhance pain relief and reduce opioid dependence. However, further research is needed to fully understand their efficacy and safety in the postoperative setting. As interest in natural remedies continues to grow, ginger and cloves stand out as promising candidates for further exploration of pain management.
One of the limitations of this study is the small sample size and dissimilarity of the groups in terms of age and type of surgery, which could affect the final evaluation of the results. Future studies should focus more on the impact of influencing factors on the results and conduct multicenter studies with larger sample sizes.
Conclusion
The results of investigating the effects of ginger, cloves, and their combination on postoperative pain in patients undergoing inguinal hernia and testicular varicocele surgery showed that these substances significantly reduced pain during recovery. The combination of cloves and ginger as analgesic agents can be used as a non-narcotic treatment option for managing mild-to-moderate pain after surgery. Further studies are needed to determine the appropriate and effective doses of clove and ginger for pain reduction.
Declarations
Acknowledgments
The authors would like to thank the research Council of Mashhad University of medical sciences for supporting the study financially.
Conflict of Interest
The authors declare no conflicts of interest.
References
- Small C, Laycock H. (2020). Acute Postoperative Pain Management. Journal of British Surgery. 107(2):e70-e80.
Publisher | Google Scholor - Fuller AM, Bharde S, Sikandar S. (2023). The Mechanisms and Management of Persistent Postsurgical Pain. Frontiers In Pain Research. 4:1154597.
Publisher | Google Scholor - Sohail R, Mathew M, Patel KK, Reddy SA, Haider Z, et al. (2023). Effects of Non-Steroidal Anti-Inflammatory Drugs (Nsaids) and Gastroprotective Nsaids on The Gastrointestinal Tract: A Narrative Review. Cureus. 15(4).
Publisher | Google Scholor - Wirth T, Lafforgue P, Pham T. (2023). NSAID: Current Limits to Prescription. Joint Bone Spine. 105685.
Publisher | Google Scholor - Cataldo G, Simone DA, Bodnar RJ. (2024). Opioids, Stress and Addiction: From Stress-Induced Analgesia to Opioid Heterodimers with Extraordinary Analgesic Efficacy and Without the Side Effects of Traditional Opioids. Addiction Neuroscience. 100168.
Publisher | Google Scholor - Gao L, Mu H, Lin Y, Wen Q, Gao P. (2023). Review of the Current Situation of Postoperative Pain and Causes of Inadequate Pain Management in Africa. Journal of Pain Research. 1767-1778.
Publisher | Google Scholor - Zhao C, Chen W, Wang D, Cong X, Zhu M, et al. (2023). Ginger (Zingiber Officinale Roscoe) Preparations for Prophylaxis of Postoperative Nausea and Vomiting: A Bayesian Network Meta-Analysis. Journal of Ethnopharmacology. 317:116791.
Publisher | Google Scholor - Boonwatcharachai K, Pongpanich S, Pripatnanont P, Oungbho K, Lerkiatbundit S, et al. (2023). Efficacy of Curcuminoids on Postoperative Pain Control After Third Molar Surgery: Multicenter Double-Blind Randomized Control Trial. Mahidol Dental Journal. 43(Suppl):S47-S56.
Publisher | Google Scholor - Pandey VK, Srivastava S, Dash KK, Singh R, Dar AH, et al. (2024). Bioactive Properties of Clove (Syzygium Aromaticum) Essential Oil Nano emulsion: A Comprehensive Review. Heliyon.
Publisher | Google Scholor - Xiang S, Jian Q, Chen W, Xu Q, Li J, et al. (2024). Pharmacodynamic Components and Mechanisms of Ginger (Zingiber Officinale) In the Prevention and Treatment of Colorectal Cancer. Journal of Ethnopharmacology. 117733.
Publisher | Google Scholor - Bekkouch O, Zengin Gk, Harnafi M, Touiss I, Khoulati A, et al. (2023). Anti-Inflammatory Study and Phytochemical Characterization of Zingiber Officinale Roscoe and Citrus Limon L. Juices and Their Formulation. ACS Omega. 8(30):26715-26724.
Publisher | Google Scholor - Oyedemi BO, Kotsia E, Stapleton PD, Gibbons S. (2019). Capsaicin and Gingerol Analogues Inhibit the Growth of Efflux-Multidrug Resistant Bacteria and R-Plasmids Conjugal Transfer. Journal of Ethnopharmacology. 245:111871.
Publisher | Google Scholor - Gao Y, Lu Y, Zhang N, Udenigwe CC, Zhang Y, et al. (2024). Preparation, Pungency and Bioactivity of Gingerols from Ginger (Zingiber Officinale Roscoe): A Review. Critical Reviews in Food Science and Nutrition. 64(9):2708-2733.
Publisher | Google Scholor - Rondanelli M, Fossari F, Vecchio V, Gasparri C, Peroni G, et al. (2020). Clinical Trials on Pain Lowering Effect of Ginger: A Narrative Review. Phytotherapy Research. 34(11):2843-2856.
Publisher | Google Scholor - Pandey VK, Srivastava S, Dash KK, Singh R, Dar AH, et al. (2024). Bioactive Properties of Clove (Syzygium Aromaticum) Essential Oil Nano emulsion: A Comprehensive Review. Heliyon. 10:e22437.
Publisher | Google Scholor - Liñán-Atero R, Aghababaei F, García SR, Hasiri Z, Ziogkas D, et al. (2024). Clove Essential Oil: Chemical Profile, Biological Activities, Encapsulation Strategies, and Food Applications. Antioxidants. 13(4):488.
Publisher | Google Scholor - Özbek ZA, Ergönül PG. (2022). Clove (Syzygium Aromaticum) And Eugenol Toxicity. Clove (Syzygium Aromaticum), 267-314.
Publisher | Google Scholor - Kheawfu K, Pikulkaew S, Rades T, Müllertz A, Okonogi S. (2018). Development And Characterization of Clove Oil Nano Emulsions and Self-Micro Emulsifying Drug Delivery Systems. Journal of Drug Delivery Science and Technology. 46:330-338.
Publisher | Google Scholor - Probert S, Cai W, Iqbal MR, Lesi OK, Haque S-U, et al. (2022). Chronic Pain as A Complication in Open Inguinal Hernia Repair: A Retrospective Study of Consenting Practice in A Single Centre. Cureus. 14(4).
Publisher | Google Scholor - Ayushi K, Danish SM, Mohammad PU. (2020). A Review on Biological and Therapeutic Uses of Syzygium Aromaticum Linn (Clove): Based on Phyto-Chemistry and Pharmacological Evidences. International Journal of Botany Studies. 5(4):33-39.
Publisher | Google Scholor - Gökalp F. (2016). A Study on The Chemical Properties of Eugenol and Eugenol Acetate, Clove Essential Oils. Sigma Journal of Engineering and Natural Sciences. 34(3):406-414.
Publisher | Google Scholor - Kaur D, Chandrul KK. (2017). Syzygium Aromaticum L (Clove): A Vital Herbal Drug Used in Periodontal Disease. Indian Journal of Pharmaceutical and Biological Research. 5(02):45-51.
Publisher | Google Scholor - Esmaeili F, Zahmatkeshan M, Yousefpoor Y, Alipanah H, Safari E, et al. (2022). Anti-Inflammatory and Anti-Nociceptive Effects of Cinnamon and Clove Essential Oils Nanogels: An In Vivo Study. BMC Complementary Medicine and Therapies. 22(1):143.
Publisher | Google Scholor - Havale R, Rao DG, Shrutha S, Tuppadmath KM, Tharay N, et al. Comparative Evaluation of Pain Perception Following Topical Application of Clove Oil, Betel Leaf Extract, Lignocaine Gel, And Ice Prior To Intraoral Injection in Children Aged 6-10 Years: A Randomized Control Study. Journal of Dental Anesthesia and Pain Medicine. 21(4):329.
Publisher | Google Scholor - Chandran R, George BP, Abrahamse H. (2020). Anti-Proliferative, Analgesic and Anti-Inflammatory Properties of Syzygium Mundagam Bark Methanol Extract. Molecules. 25(12):2900.
Publisher | Google Scholor - Ozkur M, Benlier N, Takan I, Vasileiou C, Georgakilas AG, et al. (2022). Ginger for Healthy Ageing: A Systematic Review on Current Evidence of Its Antioxidant, Anti‐Inflammatory, and Anticancer Properties. Oxidative Medicine and Cellular Longevity. (1):4748447.
Publisher | Google Scholor - Yücel Ç, Karatoprak GŞ, Açıkara ÖB, Akkol EK, Barak TH, et al. (2022). Immunomodulatory and Anti-Inflammatory Therapeutic Potential of Gingerols and Their Nano formulations. Frontiers In Pharmacology. 13:902551.
Publisher | Google Scholor - Martins LB, Rodrigues Amds, Monteze NM, Tibaes JRB, Amaral MHA, et al. (2020). Double-Blind Placebo-Controlled Randomized Clinical Trial of Ginger (Zingiber Officinale Rosc.) In The Prophylactic Treatment of Migraine. Cephalalgia. 40(1):88-95.
Publisher | Google Scholor - Kashefi F, Khajehei M, Tabatabaeichehr M, Alavinia M, Asili J. (2014). Comparison of the Effect of Ginger and Zinc Sulfate on Primary Dysmenorrhea: A Placebo-Controlled Randomized Trial. Pain Management Nursing. 15(4):826-33.
Publisher | Google Scholor - Rahnama P, Montazeri A, Huseini HF, Kianbakht S, Naseri M. (2012). Effect of Zingiber Officinale R. Rhizomes (Ginger) on Pain Relief in Primary Dysmenorrhea: A Placebo Randomized Trial. BMC Complementary and Alternative Medicine. 12:1-7.
Publisher | Google Scholor - Araya-Quintanilla F, Gutierrez-Espinoza H, Munoz-Yanez MJ, Sanchez-Montoya U, Lopez-Jeldes J. (2020). Effectiveness of Ginger on Pain and Function in Knee Osteoarthritis: A PRISMA Systematic Review and Meta-Analysis. Pain Physician. 23(2):e151.
Publisher | Google Scholor - El Tumi H, Johnson M, Dantas P, Maynard M, Tashani O. (2017). Age‐Related Changes in Pain Sensitivity in Healthy Humans: A Systematic Review with Meta‐Analysis. European Journal of Pain. 21(6):955-964.
Publisher | Google Scholor - Wettstein M, Eich W, Bieber C, Tesarz J. (2019). Pain Intensity, Disability, And Quality of Life in Patients with Chronic Low Back Pain: Does Age Matter? Pain Medicine. 20(3):464-475.
Publisher | Google Scholor