Research Article
Anatomical Landmarks of The Facial Artery About Ricketts’ Reference Plane: A Fresh Cadaveric Study
1Centro Latinoamericano de Entrenamiento Médico e Investigación (CLEMI), Bogota, Colombia.
2Instituto de Rejuvenecimiento y Optimización de Medicina Estética, ICROM Medical, Santiago de Chile.
3Medical Director, Instituto de Neurorrehabilitación y Balance Viña del Mar, Chile.
*Corresponding Author: Gladys Velazco, Centro Latinoamericano de Entrenamiento Médico e Investigación (CLEMI), Bogota, Colombia.
Citation: Velazco G., Amin M., Mercado V. (2025). Anatomical Landmarks of The Facial Artery About Ricketts’ Reference Plane: A Fresh Cadaveric Study, International Journal of Biomedical and Clinical Research, BioRes Scientia Publishers. 3(5):1-6. DOI: 10.59657/2997-6103.brs.25.066
Copyright: © 2025 Gladys Velazco, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: March 06, 2025 | Accepted: March 24, 2025 | Published: April 01, 2025
Abstract
Objective: This study aimed to establish precise topographic relationships between the facial artery (FA) and Ricketts' esthetic plane (EP) to enhance safety in minimally invasive facial procedures.
Study Design: A descriptive observational study was conducted.
Setting: For seven days in November 2024, the investigation was carried out in the cadaver labs of the Latin American Center for Research and Training in Minimally Invasive Surgery in Bogota, Colombia.
Methods: We dissected thirty freshes cadaveric hemifaces (52.4% male, 47.6% female) at CLEMI, Bogotá. After we injected red latex, we identified four key FA superficialization points through superficial dissection. We established a parallel plane to Ricketts' EP as a reference and took measurements using a calibrated Vernier caliper. We analyzed distances between FA points and the reference plane using R software.
Results: We successfully identified all four FA superficialization points in 93.3% of specimens (n=28). We measured mean distances from EP at the lateral nasal ala (3.73±0.10 cm), medial genian zone (4.64±0.18 cm), lateral labial commissure (3.66±0.08 cm), and superior nasomental groove (6.20±0.25 cm). The measurements showed an overall mean distance of 5.1 cm, with points progressing at consistent intervals (10 mm, 9 mm, and 6 mm).
Conclusion: This study provides precise measurements defining the relationship between FA superficialization points and Ricketts' EP, establishing a novel clinical reference system for safer, minimally invasive facial procedures. The consistent progression pattern of FA points relative to EP offers a reliable topographic guide for clinical practice.
Keywords: facial artery; ricketts’s plane; topographic relationship; labial commissure; nasal ala
Introduction
The facial artery (FA) represents the third branch of the external carotid artery on its anterior aspect, positioned 5 mm above the origin of the lingual artery [1,2]. The FA emits branches throughout its course to irrigate structures in cervical and facial regions [3]. Considering its extensive and variable distribution, the FA constitutes a crucial anatomical element when planning minimally invasive facial procedures [4]. Its trajectory comprises two distinct portions: the deep or cervical portion, where the hypoglossal nerve, the digastric and stylohyoid muscles, and the submandibular gland cover it. Along this path, we identify several collateral branches: the inferior palatine artery (ascending), the internal pterygoid artery, the submandibular artery, and the submental artery. The submental artery terminates in the mental region by forming an anastomosis with the mental artery, a terminal branch of the inferior dental artery [2,5].
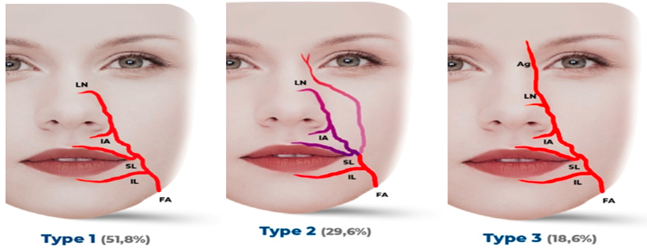
The superficial or facial portion [2,6] relates to the following muscles: platysma, depressor anguli oris, both zygomaticus muscles, common elevator of the upper lip and nasal wing. It rests upon the buccinator, caninus, and transverse nasal muscles. From its emergence at the mandibular border, the FA follows an oblique, medial, irregular, and tortuous ascent, emitting important collateral branches. A few millimeters above the mandibular border, it emits the inferior masseteric artery, ascending along the external face of the masseter muscle, distributing branches to the inferior part of the buccinator muscle. Continuing its ascent, it emits the inferior labial artery, which penetrates the thickness of the lower lip, providing circulation to muscles and glands of the region, anastomosing at the midline with its counterpart from the opposite side. The superior labial artery and its various anatomical patterns at its origin [7] emit numerous branches to the muscles and glands of the upper lip and, like the inferior labial artery, anastomose at the midline with their opposite counterparts. Between these arises the subseptal artery, which irrigates the nasal subseptum and nasal lobe [7]. A few millimeters from the nasal ala emerges the Nasal Alar artery, which irrigates the nasal ala, nasal lobe, and dorsum, maintaining anastomoses with its counterpart from the opposite side, with the subseptal and infraorbital arteries, the latter being a branch of the Ophthalmic Artery [2,7]. The termination of the FA in its ascending course presents different anatomical patterns. Lee JG et al. [8] describe three types: type 1 nasolabial pattern (51.8%), type 2 nasolabial pattern with infraorbital trunk (29.6%), and type 3 frontal or angular pattern (18.6%). In all three distribution types, the FA maintains anastomoses with branches of the ophthalmic artery and tributaries of the internal maxillary artery [2] (Figure 1).
Figure 1: Anatomical patterns of AF in its ascending course: type 1 nasolabial pattern (51.8%), type 2 nasolabial pattern with infraorbital trunk (29.6%), and type 3 frontal or angular pattern (18.6%). Ag, angular artery; IA, inferior alar artery; IL, inferior labial artery; LN, lateral nasal artery; FA, facial artery; and SL, superior labial artery. (Text with permission: Constanza AK, Marta AM, Ignacio NC, et al. (2022). Facial artery, an essential anatomy in different specialties: a review. J Otolaryngol ENT Res. 14(1):14-20. DOI: 10.15406/joentr.2022.14.00498)
The distribution of the FA, its anatomical variations, and multiple anastomoses in its superficial ascent until becoming the angular artery must be clearly and precisely understood by professionals performing minimally invasive procedures at this level [4,7-9].
It is essential to highlight the studies conducted by R. Ricketts [10], who, through cephalometric analysis, defined changes (in both men and women) in the soft tissues of the nose and lips related to skeletal growth and dental position [11]. Cephalometric results are associated with age, sex, race, ethnicity, and other physiological or physical characteristics of the study subject, allowing the determination of growth patterns and structural position [12]. Practitioners use varied cephalometric measurement techniques. We utilized four parameters in this study: the nasal tip, upper lip contour, lower lip, and soft chin tissue. With these, we established a plane called the "E Plane" (EP), which serves as a value parameter to determine the harmonic profile. The referential structures should lie behind the established line with an anteroposterior limit. Though EP demonstrates position, we have used it to reference the facial artery's inclination toward the nasal ala.
Materials and Methods
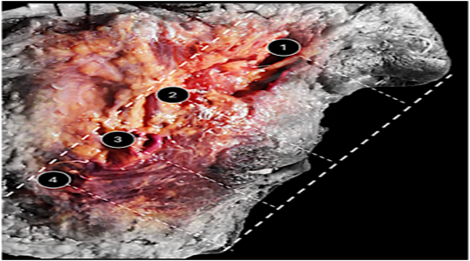
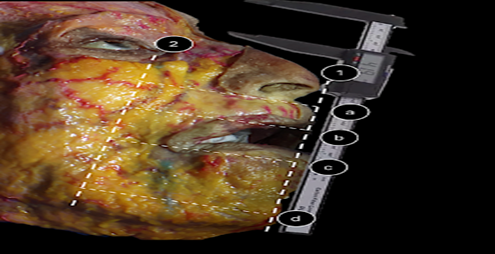
We conducted a descriptive observational study using 30 hemifaces (52.4% male, 47.6percentage female) of fresh Colombian cadavers at the Latin American Center for Research and Training in Minimally Invasive Surgery (CLEMI) in Bogotá, Colombia, in November 2024. We strictly complied with all ethical guidelines required by the Institute before obtaining authorization for the development of the study, therefore approval from an ethics committee or an institutional review board was not required. We injected red-colored latex (EPODEX) into all anatomical components. The preparation technique involved a superficial plane dissection of each hemiface to identify the points where the facial artery AF became more superficial, evidenced by the coloration of the structure, establishing these as reference points for the exposure of the artery. The dissection remained in the plane of the deep dermis, just below the superficial fat, with photographic documentation of each point. We always used digital photography to verify the inner canthal line and maintain exact parallelism with the EP. We corrected any misalignment in this relationship before taking the measurement. The line of the inner corner of the eye was traced and drawn after confirming its exact parallelism with EP. Thus, the specific objective was to draw a parallel plane (PP) to the EP (calculable in cadavers since the cephalometric points remain constant), which was coincident with the trajectory of the AF, and for this, we used as an anthropometric reference a line from the inner corner of the eye to the mandibular edge, as we had previously proposed. Our team recorded the AF's superficial dissection point measurements along the PP. We employed a dual-caliper technique, using two calibrated JESWO Vernier calipers. We anchored the first caliper to the EP and used the second to measure distances, tracking the AF's superficial points with the PP as our guide. Dissection of the AF from the mandibular border to the nasal ala defined four points of surface elevation: 1) lateral to the nasal ala, 2) medial extension of the genital area, 3) lateral to the labial commissure, and 4) superior extension of the nasomental groove. For statistical analysis, we considered only dissections that allowed definitive access to all four points, and we took measurements anthropometrically on the anatomical specimen (Figures 2,3).
Figure 2: Contrast photography of the performed dissection, showing the defined FA points 1. Lateral to nasal ala, 2. Medial extension of the genian zone, 3. Lateral to labial commissure, 4. Superior extension of nasomental groove, with the tangential tracing of arterial elevation.
Figure 3: Image illustrating the position used for respective measurements. 1) We placed the Vernier caliper exactly on Ricketts's aesthetic plane. 2) The line parallels the RP with the inner canthus as an anthropometric reference. Specific superficialization points: lateral to nasal ala (a), medial extension of genian zone (b), lateral to labial commissure (c), superior extension of nasomental groove (d).
Statistical Analysis
We analyzed data using R software (version 4.1.0, R Foundation for Statistical Computing, Vienna, Austria). We included measurements from all 28 specimens and utilized packages including ggplot2, dplyr, and tidyr for data visualization and analysis. We calculated descriptive statistics for each anatomical reference point, including means, standard deviations, and ranges. We examined distribution patterns through boxplots and density plots to assess measurement variability and identify potential outliers. We standardized all measurements in centimeters and excluded cases with missing values from specific analyses. We focused the study on the four key anatomical reference points, comprehensively assessing FA superficial elevation points. We present results as mean ± standard deviation, with ranges indicating minimum and maximum values for each measurement point.
Results
Of the 30 dissected hemifaces, in 28 (93.3%), we achieved superficial visualization of the FA at all four reference points. This enabled the calculation of the linear distance between these points and the EP, following the PP line for linear measurement. Measurements were obtained at all four established points from the 28 hemifaces, totaling 112 measurements, and an average was figured for each point. We highlight the significant coincidence of the PP with the ascending course of the FA in parallel projection with the EP. This allowed for exact and linear measurements based on a line drawn from the PP that intersected the FA's superficialization point and was perpendicular to both planes. A line connecting the measurement results at the four defined points revealed a periodic tangent to the mandibular plane, which showed a slight deviation from the parallel PP and EP. The obtained distances allowed us to calculate X̄ = 5.11 cm (Table 1).
Table 1: Illustrates the distances between four anatomical reference points and the reference plane in 28 specimens.
| Anatomical Reference Point | N | Mean ± SD (cm) | Range (cm) |
| 1.a Lateral to nasal ala | 28 | 3.73 ± 0.10 | 3.50 - 3.80 |
| 2.b Medial genian zone | 28 | 4.64 ± 0.18 | 4.00 - 4.80 |
| 3.c Lateral to labial commissure | 28 | 3.66 ± 0.08 | 3.50 - 3.70 |
| 4.d Superior nasomental groove | 28 | 6.20 ± 0.25 | 5.00 - 6.30 |
| Mean Value (X̄) | 5.1 |
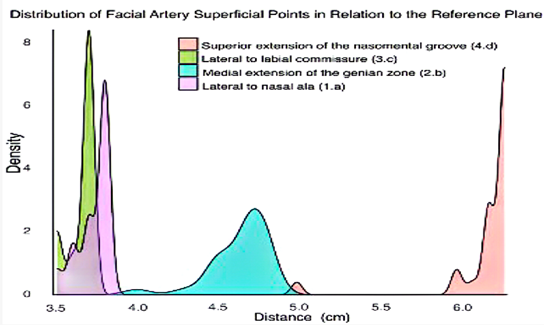
The lateral nasal ala (1.a) and lateral labial commissure (3.c) showed similar mean distances (3.73 ± 0.10 cm and 3.66 ± 0.08 cm, respectively), while the medial genian zone (2.b) presented an intermediate value (4.64 ± 0.18 cm). The superior nasomental groove (4.d) demonstrated the most significant distance (6.20 ± 0.25 cm) and widest range (5.00 - 6.30 cm). All measurements showed consistent patterns with relatively small standard deviations. The overall mean value (X̄) of 5.1 cm represents the average measurement across all reference points, providing a central reference value for the facial artery's course. All measurements showed consistent patterns with relatively small standard deviations. Our measurements revealed increasing variations toward the superior mentonian line of the nasomentonian groove when we analyzed distances between the previously defined FA points and the EP. We found varying distances between points: 10 mm separated points 1 and 2, 9 mm separated points 2 and 3-, and 6-mm separated points 3 and 4, yielding a mean of 5.1 cm and suggesting an equitable linear distribution (Figure 4). These findings allow clinicians to predict FA superficial points in relation to the EP from a topographic perspective.
Figure 4: The density distribution reveals distinct clustering patterns for each anatomical point, with the superior extension of the nasomental groove (4.d) showing the most significant distance from the reference plane at approximately 6.0-6.3 cm. The lateral to nasal ala (1.a) and lateral to labial commissure (3.c) points demonstrate similar distributions around 3.5-3.8 cm, while the medial extension of the genian zone (2.b) shows a broader distribution centered around 4.5-4.8 cm.
Discussion
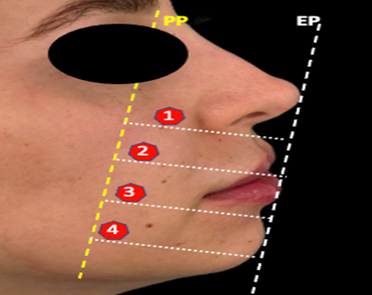
Scientists recognize the FA and its facial and cervical distribution for its variability and multiple anastomoses [2,9,13,14]. Practitioners must consider anatomical landmarks and evaluate procedures topographically to reduce vascular damage risk, while accounting for the AF's possible course [15]. Recent publications demonstrate an increasing trend in vascular complications following hyaluronic acid and other filler injections [15]. Even with knowledge of the risk zones for vascular obstruction complications, minimally invasive facial procedures continue to be analyzed to increase safety [16,17]. The dissection study presented here demonstrates that the FA at the mentonian and nasogenian zones in its four defined points and EP show good correlation, with minimal variations compared to published measurements using other anatomical landmarks [2, 8, 9, 16,18 -20]. We recognize potential differences between planes measured in cadavers and patients due to structural changes that soft tissues undergo during maintenance and refrigeration techniques. Our measurements may contain some degree of inaccuracy, commonly occurring in techniques using a variable reference like EP (although each person's EP is unique, the Vernie's placement in this plane allowed for a sufficient measurement). However, even considering these weaknesses of the study, we maintain that these findings may provide a useful anatomical reference for localizing AF when performing different procedures at this level. We suggest maintaining permanent knowledge of FA distribution and, ideally, anatomical training of its course, thus allowing confident management of all territories potentially receiving minimally invasive procedures, as it is known that vascular complications can have devastating consequences [13,15,18]. The results of measurements between the four superficialization points of the FA and Ricketts' aesthetic plane may contribute to maximizing safety and minimizing risks for different procedures performed at the facial level (Figure 5).
Figure 5: Clinicians should consider the projection of the four FA points about the PP and EP as a topographic clinical reference before performing procedures at this level. (PP, yellow dashed lines, represents the parallel plane from the internal orbital edge to the mandibular rim; EP, white dashed lines, shows Ricketts’s aesthetic plane; red points 1 to 4 indicate the clinical location of the FA.).
Conclusion
Our study established precise measurements between four points of the FA and Ricketts' EP; practitioners should consider this anatomical-topographic relationship as a guiding element before performing minimally invasive procedures.
Declarations
Author Contributions
Gladys Velazco: conception, writing, data collection, analysis, revisions.
Marta Amin: data collection, revisions, supervision.
Víctor Mercado: writing, data collection, revisions, supervision.
Ignacio Novoa: conception, writing, statistical analysis, revisions, supervision.
Acknowledgments
The authors would like to thank the Latin American Center for Research and Training in Minimally Invasive Surgery (CLEMI), Bogotá, Colombia, for allowing us to conduct this study at their facilities. We would especially like to thank thanatologist Holman Anaya for his valuable contribution.
Conflicts of Interest
The authors declare no conflicts of interest in the conduct of this study.
Ethical Standards
The authors declare compliance with all ethical protocols required by CLEMI to carry out this study.
Funding Source
The research presented in this publication was not funded.
References
- Zümre, Ö., Salbacak, A., Çiçekcibaşi, A. E., Tuncer, I., Seker, M. (2005). Investigation of the Bifurcation Level of The Common Carotid Artery and Variations of The Branches of The External Carotid Artery in Human Fetuses. Annals of Anatomy-Anatomischer Anzeiger, 187(4):361-369.
Publisher | Google Scholor - Constanza, A. K., Marta, A. M., Ignacio, N. C. (2022). Facial Artery, An Essential Anatomy in Different Specialties: A Review. J Otolaryngol ENT Res, 14(1):14-20.
Publisher | Google Scholor - Niranjan, N. S. (1988). An Anatomical Study of The Facial Artery. Annals of Plastic Surgery, 21(1):14-22.
Publisher | Google Scholor - Yang, H. M., Lee, J. G., Hu, K. S., Gil, Y. C., Choi, Y. J., et al. (2014). New Anatomical Insights on The Course and Branching Patterns of The Facial Artery: Clinical Implications of Injectable Treatments to The Nasolabial Fold and Nasojugal Groove. Plastic And Reconstructive Surgery, 133(5):1077-1082.
Publisher | Google Scholor - Gocmen-Mas, N., Edizer, M., Keles, N., Aksu, F., Magden, O., et al. (2015). Morphometrical Aspect on Angular Branch of Facial Artery. Journal of Craniofacial Surgery, 26(3):933-936.
Publisher | Google Scholor - Wortsman, X., Wortsman, J. (2010). Clinical Usefulness of Variable-Frequency Ultrasound in Localized Lesions of The Skin. Journal of the American Academy of Dermatology, 62(2):247-256.
Publisher | Google Scholor - Cotofana, S., Pretterklieber, B., Lucius, R., Frank, K., Haas, M., et al. (2017). Distribution Pattern of The Superior and Inferior Labial Arteries: Impact for Safe Upper and Lower Lip Augmentation Procedures. Plastic and Reconstructive Surgery, 139(5):1075-1082.
Publisher | Google Scholor - Lee, J. G., Yang, H. M., Choi, Y. J., Favero, V., Kim, Y. S., et al. (2015). Facial Arterial Depth and Relationship with The Facial Musculature Layer. Plastic and Reconstructive Surgery, 135(2):437-444.
Publisher | Google Scholor - von Arx, T., Tamura, K., Oba, Y., Lozanoff, S. (2018). The Face-A Vascular Perspective. Swiss Dental Journal SSO-Science and Clinical Topics, 128(5):382-392.
Publisher | Google Scholor - Morroy, R. R. (1960). Cephalometric Synthesis. Am J Orthod, 647-673.
Publisher | Google Scholor - Formby, W. A., Nanda, R. S., Currier, G. F. (1994). Longitudinal Changes in The Adult Facial Profile. American Journal of Orthodontics and Dentofacial Orthopedics, 105(5):464-476.
Publisher | Google Scholor - De Smit, A., Dermaut, L. (1984). Soft-Tissue Profile Preference. American Journal of Orthodontics, 86(1):67-73.
Publisher | Google Scholor - Ashton, M. W., Taylor, G. I., Corlett, R. J. (2018). The Role of Anastomotic Vessels in Controlling Tissue Viability and Defining Tissue Necrosis with Special Reference to Complications Following Injection of Hyaluronic Acid Fillers. Plastic and Reconstructive Surgery, 141(6):818e-830e.
Publisher | Google Scholor - Loukas, M., Hullett, J., Louis, R. G., Kapos, T., Knight, J., et al. (2006). A Detailed Observation of Variations of The Facial Artery, With Emphasis on The Superior Labial Artery. Surgical and Radiologic Anatomy, 28:316-324.
Publisher | Google Scholor - Doyon, V. C., Liu, C., Fitzgerald, R., Humphrey, S., Jones, D., et al. (2024). Update on Blindness from Filler: Review of Prognostic Factors, Management Approaches, And A Century of Published Cases. Aesthetic Surgery Journal, 44(10):1091-1104.
Publisher | Google Scholor - Scheuer III, J. F., Sieber, D. A., Pezeshk, R. A., Gassman, A. A., Campbell, C. F., et al. (2017). Facial Danger Zones: Techniques to Maximize Safety During Soft-Tissue Filler Injections. Plastic and Reconstructive Surgery, 139(5):1103-1108.
Publisher | Google Scholor - Ten, B., Kara, T., Kaya, T. İ., Yılmaz, M. A., Temel, G., et al. (2021). Evaluation of Facial Artery Course Variations and Depth by Doppler Ultrasonography. Journal of Cosmetic Dermatology, 20(7):2247-2258.
Publisher | Google Scholor - Tansatit, T., Moon, H. J., Rungsawang, C., Jitaree, B., Uruwan, S., et al. (2016). Safe Planes for Injection Rhinoplasty: A Histological Analysis of Midline Longitudinal Sections of The Asian Nose. Aesthetic Plastic Surgery, 40:236-244.
Publisher | Google Scholor - Nguyen, V. H., Cheng-Kuan, L., Nguyen, T. A., Cai, T. H. N. T. (2023). Facial Artery: Anatomical Variations in The Perioral Region in Cadavers. Archives of Craniofacial Surgery, 24(6):266.
Publisher | Google Scholor - Fakoya, A. O., Hohman, M. H., Westbrook, K. E., Varacallo, M. A. (2024). Anatomy, Head and Neck: Facial Muscles. StatPearls Publishing.
Publisher | Google Scholor