Review Article
Analysis of The Surgical Treatment of Diaphyseal Fractures of the Tibia with Interfragmentary Screws in A Reference Hospital in Brazil
- Henrique Luiz Fidelis de Farias 1
- Bianca Gabriella de oliveira 2*
- João Henrique Meneses Xavier 3
- Filippe de Macedo Ribeiro 4
- Ricardo Filgueiras Da Matta 5
1Doctor from Uniceplac - DF (Centro Universitário do Planalto Central Apparecido dos Santos) and R3 Resident in orthopedics and traumatology at the Hospital Regional de Ceilândia–DF.
2Medical Student at the University of Salvador-UNIFACS, Salvador, BA, Brazil.
3Doctor from the University of Rio Verde - Aparecida Campus and medical resident from ESCS at HRC.
4Doctor by IMEPAC 2018/HRC.
5Professor of the discipline of Practice in Orthopedics and Traumatology of the Medicine course at the Catholic University of Brasília. Preceptor of the Medical Residency Program in Orthopedics and Traumatology at the Hospital Regional da Ceilândia. Orthopedist at Hospital São Francisco, Ceilândia.
*Corresponding Author: Bianca Gabriella de oliveira, Medical Student at the University of Salvador-UNIFACS, Salvador, BA, Brazil.
Citation: H. L. F. D. Farias, B. G. D. oliveira, J. H. M. Xavier, F. D. M. Ribeiro, R. F. D. Matta (2024). The Importance of Assisted Weight Training in Lumbosciatalgia. Journal of Clinical Rheumatology and Arthritis, BioRes Scientia Publishers. 2(1):1-6. DOI: 10.59657/2993-6977.brs.24.014
Copyright: © 2024 Bianca Gabriella De Oliveira, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: March 26, 2024 | Accepted: April 12, 2024 | Published: April 17, 2024
Abstract
This retrospective cohort study evaluated the surgical treatment of tibial shaft fractures with interfragmentary screws in nine patients who underwent the procedure at the Hospital Regional de Ceilândia. The patient cohort was predominantly characterized by individuals with a mean age of 41.8 years. The bone union rate was 88% of cases with an average union time of 96.42 days. Six patients had no complications and two patients had possible injuries to the peroneal nerve and one case required re-approach. Finally, it is noteworthy that no infections, delayed union or pseudarthrosis were found in the evolutions and outpatient records of infections in the observed patients.
Keywords: tibial shaft fracture; surgical treatment; interfragmentary screws
Introduction
The fracture of the diaphysis of the bones of the lower leg poses challenges in terms of therapeutic management, since anatomically, it is the most prevalent long bone fracture and is more susceptible to delayed healing and non-union due to its poor blood supply. Studies show that the standard treatment for closed tibial shaft fractures is intramedullary fixation and subsequent early loading. After closed reduction, alignment must be maintained so that there is less than one centimeter of shortening, angulation is limited to less than 5° and rotational deformity is limited to 5° or less [1]. Recovery from these fractures can be slow, with temporary or permanent withdrawal of the patient from their daily activities and the possibility of permanent deformity and definitive functional alterations [2,3,4,5]. Approximately 6 to 10% of tibial fractures are open, 70% of which occur in isolation, while 30% are associated with an ipsilateral fracture of the fibula. Animal and human studies have shown the benefit of controlled interfragmentary movement in fractures. Fracture healing is a complex process that occurs through primary healing, secondary healing or a combination of both in part, based on the range and type of movement between the fragments [11]. Diaphyseal tibial fractures may require plate fixation for proper healing to occur. Currently, there is no consensus on the number of screws required for proper fixation or the ideal placement of the screws within the plate. However, the number and location of the screws have implications for the mechanical environment at the fracture site and, consequently, the bone healing response: The interfragmentary movement achieved with a specific plate and screw construction can provoke signals that influence cell type differentiation, which in turn affects how well the fracture heals [12].
Patients treated with interfragmentary screws were reviewed at an average of 2 years after surgery and excellent results, with anatomical healing, were achieved in 30 patients (55%) and good results with less than 5 degrees of misalignment in 6 (11%). There was a highly statistically significant association of satisfactory results with the initial anatomical operative reduction of the fracture, a ratio of fracture length to tibial diameter of 2 or more and the absence of comminution. The orientation and number of screws, the delay in the operation, the degree of initial fracture displacement and the patient's age were not shown to affect the outcome [13]. In another study, 10 patients underwent interfragmentary screws and external fixation for unilateral tibial shaft fractures. Anatomical reduction was achieved in all cases and uncomplicated bone union occurred in nine patients with a mean union time of 122 (SD 20) days. One patient delayed union and the fracture disunited. A tract sepsis rate of 20% was found. The risk of infection, the demanding follow-up and the availability of better methods do not allow this technique to be recommended in the routine treatment of closed diaphyseal tibial fractures [14]. Although interfragmentary screws seem to block the necessary interfragmentary movement, we see callus formation as a sign of secondary fracture healing. The interfragmentary screw osteosynthesis construct appears to be more stable and less flexible than the single bridge plating, leading to faster fracture healing. Interfragmentary screws can help control and limit interfragmentary movement in certain cases [15]. Therefore, the primary objective of this study was to evaluate the bone healing rate of diaphyseal tibial fractures surgically treated with interfragmentary screws. The secondary objectives were divided into: To evaluate the average healing time of the treated fractures; to investigate the rate of complications related to surgical treatment and to analyze the predictive factors of successful surgical treatment.
Methodology
This is a retrospective observational analytical longitudinal cohort study which included patients who underwent surgical treatment of diaphyseal tibial fractures with interfragmentary screws. The treatments were carried out at the Ceilândia Regional Hospital, in the Federal District, between January 2013 and May 2023, after the patient had signed an informed consent form. The ICF( TCLE) consists of the individual's choice to take part in the research, free from coercion by the researcher involved, other professionals, their family, friends or society itself. Some authors emphasize that consent is an active active authorization and not simply passive agreement. It is made up of three basic elements: competence or capacity, information and consent (according to CNS Resolution 196/96).
Informed consent for research purposes is made up of eight basic elements elements:
- Information about what the research is, objectives, duration of involvement and types of procedures, highlighting which are experimental;
- Risks and discomforts, including possible embarrassment;
- Benefits;
- Alternatives, if any;
- Confidentiality;
- Compensation, if any, for the treatment, should any damage occur;
- Identification of a contact person;
- Voluntary acceptance and the possibility of abandonment without restrictions or consequences
Another 6 optional elements can be added to the Consent Form Informed Consent Form:
- Information that unforeseen risks may occur;
- What are the circumstances for withdrawing a patient from the study; 3. What are the additional costs generated by their participation;
- Information about premature discontinuation;
- Guarantee of the provision of new information that is generated during the course of the study;
- The size of the sample to be studied.
The following ethical principles were respected throughout the research
Beneficence/non-maleficence: The first principle to be considered in this project will be that of beneficence/non-maleficence (also known as benefit/non-maleficence). The benefit (and non-maleficence) of the patient and of society has always been the main reason for practicing professions that involve people's health - "avoiding harm". Aiming to offer the best treatment to their patient, both in terms of technique and in terms of recognizing the patient's physical, psychological or social needs. A professional must, above all, want the best for their patient, to restore their health, to prevent an illness, or to promote their health.
Autonomy: The second principle to be used as a "tool" for dealing with ethical issues is the principle of autonomy. According to this principle, people have "freedom of decision" over their lives. Autonomy is a person's capacity for self-determination, i.e. the extent to which they can manage their own will, free from the influence of other people. It includes the right to be sufficiently informed about the procedure that the professional is going to adopt. For respect for people's autonomy to be possible, two conditions are fundamental: freedom and information. This means that, in the first instance, the person must be free to decide. To do this, they must be free from external pressures, because any kind of pressure or subordination makes it difficult to express autonomy. At times, people find it difficult to express their freedom. In these cases, we say that their autonomy is limited.
Justice: The third principle to be considered will be the principle of justice. This refers to equal treatment and the fair distribution of state funds for health, research, etc. According to the principle of justice, everyone's rights must be respected impartially. A decision that the sample size was defined in advance, taking into account the total number of patients undergoing surgical treatment, a total of thirty [30]. patients, of whom nine [09] agreed to take part in the study. All the surgical procedures were carried out by the same orthopedic team, always under the same pre- and post-surgical protocols. The first included X-ray assessment to analyze the fracture trace and the second included outpatient follow-up, use of a splint and orthopedic boot for about a month.
The participants were invited to the Ceilândia Regional Hospital, where they were given more information about the research project and signed an informed consent form.
Inclusion and Exclusion Criteria
Five inclusion criteria were defined in order to collect the research data:
- Diaphyseal fracture of the tibia with an oblique or spiral trace.
- The fracture trace must be at least twice the length of the diaphysis diameter.
- Ability to follow up and adhere to the rehabilitation protocol.
- Patients aged between 18 and 70 years.
Exclusion criteria were patients with:
- A diaphyseal fracture of the tibia with a transverse trace.
- Fractures with significant bone loss.
- Pathological fractures.
- Fractures associated with significant neurovascular lesions.
Risks and Benefits
The following risks were defined in this study:
Data privacy and confidentiality: When accessing patients' physical and electronic medical records, there is a risk of data privacy and confidentiality being violated. The researchers used a personal password on a private computer with access restricted to the principal investigator and there was no cloud storage of data.
Selection bias: As this is a retrospective study, the researchers may be subject to selection bias when choosing which medical records to include in the analysis. The selection was well defined and justified to avoid distorting the results.
Information bias: The data contained in the medical records may be subject to documentation errors or missing information, which could lead to information bias. The researchers carried out rigorous data collection and validated the accuracy of the information.
Limited generalizability: The results obtained in a single treatment center (Hospital Regional de Ceilândia) may have limitations in generalizability to other populations or health centers. This research can be considered lower level evidence than randomized multicentre studies.
It was considered beneficial that this retrospective cohort study could provide information on the clinical and functional results of the surgical treatment of diaphyseal tibial fractures with interfragmentary screws in patients treated at the Ceilândia Regional Hospital from January 2013 to May 2023. The results could help evaluate the efficacy and safety of this procedure and provide input for future clinical decisions and research in the field of orthopaedics.
Data Collection and Analysis Methodology
Firstly, data was collected from each patient's medical records and outpatient assessment. Next, a data description table was drawn up (tab.1), which included: patient's age during hospitalization; date of fracture; date of surgery; healing; days until healing; occurrence of complications; occurrence of new procedures and observations. Finally, a descriptive analysis was carried out to evaluate the study hypotheses and the primary and secondary outcomes.
Results
In this study, the patient cohort was characterized by individuals with a mean age of 41.8 years (minimum age: 32 years; maximum age: 63 years) (Table 1). The sample of patients for this study who underwent treatment with the interfragmentary screw technique had spiral or oblique fractures. The results of the retrospective study of patients with diaphyseal tibial fractures who were treated with the interfragmentary screw technique are shown in Table 1.
Table 1: General characteristics of the study participants
| Paciente | Age (hospitalization) | Date of fracture | Surgery date | Consolidation | ∆t(days) Consolidation | Complications |
| P1 | 41 | 16/092013 | 23/09/2013 | Yes | 90 | No |
| P2 | 43 | 29/05/2014 | 06/06/2014 | Yes | 90 | No |
| P3 | 44 | 08/08/2015 | 14/08/2015 | Yes | 90 | Fibula nerve injury* |
| P4 | 18 | 01/03/2016 | 01/03/2016 | Yes | 150 | No |
| P5 | 50 | 12/02/2019 | 12/02/2019 | No | - | Reapproach |
| P6 | 42 | 24/02/2023 | 06/03/2023 | Yes | - | Peroneal nerve injury** |
| P7 | 63 | 18/03/2023 | 27/03/2023 | Yes | 90 | No |
| P8 | 32 | 24/04/2023 | 02/05/2023 | Yes | 75 | No |
| P9 | 44 | 26/04/2023 | 02/05/2023 | Yes | 90 | No |
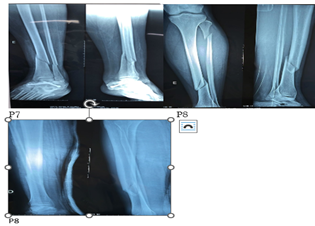
Analisou-se as radiografias em Ap e perfil dos participantes do estudo que mostram traço de fratura diafisária de tíbia oblíqua. Ap and lateral radiographs of the study participants were analyzed, showing a trace of an oblique tibial diaphyseal fracture.
Figure 1: Ap and lateral radiographs of participants P7, P8 and P9 – Preoperative
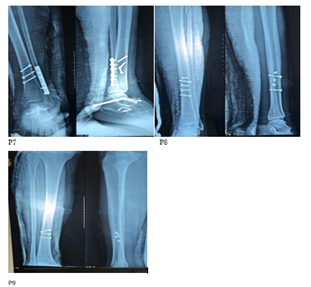
Figure 2: Ap and lateral radiographs of participants P8 and P9 - Post-surgery, A consolidação das fraturas após realização do procedimento cirúrgico foi alcançada em 88% dos pacientes analisados (fig.2). Consolidation of the fractures after the surgical procedure was performed was achieved in 88% of the patients analyzed (fig.2).
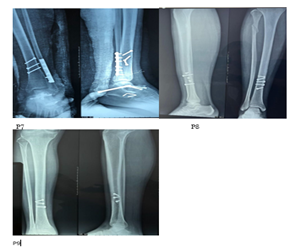
Figure 3:Radiographs of patients P7, P8 and P9 in Ap and profile showing signs of healing.
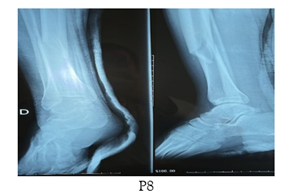
Figure 4: Ap and profile radiograph of participant P8 - Post Consolidation Patient P5 did not heal properly due to the new trauma he was subjected to, stepping without medical authorization and, consequently, falling and requiring a new surgical approach with plates and screws.
Discussion
The average healing time for diaphyseal tibial fractures, using the technique with interfragmentary screws and external fixation, can be 122 days (15). In this study, we used data from 7 patients from the list analyzed, because patient P5 underwent a new surgical procedure and patient P6 did not have adequate outpatient follow-up to estimate the healing time. The data showed that the average healing time was 96.42 days, with the exception of P4, who had a healing time of 150 days (minimum time: 75 days; maximum time: 150). Epiphyseal fractures and dislocations occur as a result of forces applied indirectly to the site of the affected lower limb. Direct trauma produces transverse, simple oblique or comminuted fractures. The torsion mechanism with angulation can result in a long oblique or spiral fracture [6,7,8,9]. Complications found in these fractures in adults, such as infection, delayed healing and pseudarthrosis, are less frequent in children, but the risk of compartment syndromes is an eventuality that requires attention, especially in non-invasive procedures with plaster immobilization [10].
As for surgical treatment with interfragmentary screws, fixation of the diaphyseal fracture of the tibia with interfragmentary screws is carried out as a non-invasive procedure, with anatomical reduction and absolute stability. Normally, bone callus does not form, and absolute stability promotes healing by remodeling the osteon - the very functional unit of the bone that promotes healing. Patients with diaphyseal tibial fractures who have undergone surgery may present complications such as infection, delayed healing, pseudoarthrosis and others (11). The results show that six patients had no complications. Patients P3 and P6 had possible injuries to the peroneal nerve and P5 needed reapproachment. However, the re-approach was due to a new trauma, which has no correlation with the surgical technique. It should be noted that patient P1 underwent a new surgical approach due to high-energy trauma to the tibia. With regard to complications, it should also be noted that the evolution and outpatient records of infections, delayed consolidation or pseudoarthrosis were not found in the patients observed.
Conclusion
In conclusion, the first finding was that the bone healing rate of diaphyseal tibial fractures treated surgically with interfragmentary screws was as expected. Although one patient required reoperation. A second, very clear finding was that the average healing time was within the expected time, with a low complication rate and predictive factors of successful surgical treatment. Finally, we would like to point out that one of the difficulties of the study was access to the radiographs of all the patients and we suggest that further research be carried out into the surgical treatment of diaphyseal tibial fractures with interfragmentary screws in order to expand the literature on the subject.
Conclusion
In conclusion, the first finding was that the bone healing rate of diaphyseal tibial fractures treated surgically with interfragmentary screws was as expected. Although one patient required reoperation. A second, very clear finding was that the average healing time was within the expected time, with a low complication rate and predictive factors of successful surgical treatment. Finally, we would like to point out that one of the difficulties of the study was access to the radiographs of all the patients and we suggest that further research be carried out into the surgical treatment of diaphyseal tibial fractures with interfragmentary screws in order to expand the literature on the subject.
References
- El-Sayed, Mohamed, and Ashraf Atef. “Management of simple (types A and B) closed tibial shaft fractures using percutaneous lag-screw fixation and Ilizarov external fixation in adults.” International orthopaedics, 36(10):2133-2138.
| Google Scholor - Falavinha R.S, Costa C. A. (1997). Placa e parafuso no tratamento das fraturas da diáfise dos ossos da perna. Rev Bras Ortop, 32(6).
Publisher | Google Scholor - Bengner V, Ekbom T, Johnell T. et al. (1990). Incidence of femoral and tibial shaft fractures. Acta Orthop Scand, 61:251-254.
Publisher | Google Scholor - Punno R.M, Vaughan J.J, Stetten M.L. et al. (1991). Long-term effects of tibial angular mal union on the knee and ankle joints. J Orthop Trauma, 5:247-254.
Publisher | Google Scholor - Grazier K.L, Holbrook T.L, Kelsey J.L. et al. (1984). The frequency of ocurrence, impact and cost of musculoskeletal conditions in the United States, Chicago. American Academy of Orthopaedic Surgeons.
Publisher | Google Scholor - Worlock P, Stower M. (1986). Fracture patterns in Nottingham children. J Pediatr Orthop, 6:656-60.
Publisher | Google Scholor - Rockwood CA Jr. (1996). Fractures in children. 4rd ed. Philadelphia: Lippincott.
Publisher | Google Scholor - Beaty JH, Kasser JR, editors. (2004). Rockwood and Wilkins fraturas em crianças. Tradução de Mirtes Frange de Oliveira Pinheiro. 5 ed. São Paulo: Manole.
Publisher | Google Scholor - Koval KJ, Zuckerman JD. (2006). Handbook of fractures. 3rd ed. New York: Lippincott Willians & Wilkins.
Publisher | Google Scholor - Santili C, Gomes CMO, Akkari M, Waisberg G, Braga SR. et.al. (2010). Fraturas da diáfise da tíbia em crianças. Acta Ortop Bras, 18(1):44-48.
Publisher | Google Scholor - Ziran, Navid, et al. (2021).
Publisher | Google Scholor - Travascio, Francesco et al. “Mechanical performance and implications on bone healing of different screw configurations for plate fixation of diaphyseal tibia fractures: a computational study.” European journal of orthopaedic surgery & traumatology: orthopedie traumatology, 31(1):121-130.
Publisher | Google Scholor - Dent, J A, and W a Hadden. “Interfragmentary screw fixation of fractures of the tibial shaft.” Injury, 18(1):28-32.
Publisher | Google Scholor - Grevitt, M P. “Treatment of fractures of the tibial shaft with inter-fragmentary screws and external fixation.” Journal of the Royal Army Medical Corps,138(1):33-35.
Publisher | Google Scholor - Horn, C et al. “Combination of interfragmentary screws and locking plates in distal meta-diaphyseal fractures of the tibia: a retrospective, single-centre pilot study.” Injuryvol, 42(10):1031-1037.
Publisher | Google Scholor