Case Report
Acute Kidney Injury After Double-J Stent Placement in A Diabetic Patient with Multiple Comorbidities: A Case Report
1Medical student, Washington University of Health and Science, Belize.
2PhD in Biology Curriculum and Strategic Teaching, Assistant Dean for Academic Affairs and Scientific Research, Global University College of Science and Health. 3Pediatric Urologist, Jenin Governmental Hospital, Palestine.
*Corresponding Author: Ansam Aljaghoub, Medical student, Washington University of Health and Science, Belize.
Citation: Aljaghoub A, Alassali A, Quraish A. (2024). Acute Kidney Injury After Double-J Stent Placement in A Diabetic Patient with Multiple Comorbidities: A Case Report, Clinical Case Reports and Studies, BioRes Scientia Publishers. 7(5):1-11. DOI: 10.59657/2837-2565.brs.24.200
Copyright: © 2024 Ansam Aljaghoub, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: November 05, 2024 | Accepted: November 19, 2024 | Published: November 28, 2024
Abstract
Introduction: Acute kidney injury is considered a potential rare complication of Ureteral stent placement, but it can happen, especially in patients with multiple comorbidities.
Case Presentation: We report a case of a 71-year-old male patient with a history of diabetes mellitus (DM), hypertension (HTN), and dyslipidemia, who was also suffering from ischemic heart disease treated by percutaneous coronary intervention (PCI) and stenting two months ago. The patient presented with obstructive pyelonephritis, experiencing stabbing flank pain and hematuria for 4 days. Initial investigations revealed obstructive uropathy due to a left ureteric stone, and laboratory results indicated a creatinine level of 3.1 mg/dL. Despite ongoing prasugrel (antiplatelet) medication, an urgent double-J (DJ) stent placement was attempted but failed due to severe obstruction. Hence, the plan was to discontinue prasugrel and start enoxaparin for 5 days, during which time he received intravenous antibiotics and fluids, showing progressive improvement in creatinine levels. Following the second DJ stent placement surgery, the patient experienced worsening bilateral flank pain, nausea, vomiting, and a significant increase in creatinine, peaking at 4.31 mg/dL. The patient had full management inclusive of volume and electrolyte assessment. A gradual improvement in kidney function was observed over the following weeks.
Conclusion: This case highlights the interplay between stent placement, antiplatelet management, and AKI risk in a diabetic elderly patient, by which we hope to underscore the need for careful perioperative planning and monitoring.
Keywords: acute kidney injury; double-j stent placement; diabetic patient; multiple comorbidities
Introduction
DJ stent placement is a crucial urological intervention to maintain ureteral patency [6]. This could be employed in the setting of ureteral obstruction or as a part of other endourological procedures [11]. Though generally safe, complications like infection, migration, encrustation, and less common AKI can occur [1].
AKI is a sudden decrease in GFR, usually reversible, and results in an increase in the end-product of nitrogen metabolism, such as urea and creatinine [2]. The Kidney Disease, Improving Global Outcomes (KDIGO) defines AKI as any of the following: [5]
- Increase in serum creatinine by ≥ 0.3 mg/dL or more within 48 hours or
- Increase in serum creatinine to ≥ 1.5 times baseline or more within the last 7 days or
- Urine output less than 0.5 mL/kg/h for 6 hours
Diabetics are more predisposed to AKI due to pre-existing damages in the micro-vessels, impaired renal autoregulation, and increased risk of infections and nephrotoxicity. Comorbid conditions like hypertension and ischemic heart disease are more likely to further escalate the risk of developing AKI in this patient [3,4].
Recent studies have shown that acute kidney injury (AKI) is more prevalent in individuals with diabetes, especially those with multiple comorbidities. Interestingly, among 36,106 patients from the SWEDEHEART register who underwent primary isolated CABG between 2003 and 2013, AKI was more common in people with a diagnosis of type 1 diabetes (32%) than patients with type 2 diabetes (20%) in comparison with patients without diabetes (13%) [12]. Furthermore, in a registry study from Taiwan. Incidence of AKI was significantly higher in older-old patients compared to old and young groups. Cardiovascular comorbidities were shown to increase the risk of AKI [12].
The importance of this case report lies in the reporting of AKI occurrence following the placement of a double-J stent in a diabetic patient with a complicated medical history that includes hypertension, dyslipidemia, and ischemic heart disease. Such comorbidities make the risk of AKI higher, demonstrating the complex interplay of factors that must be meticulously managed in high-risk patients. The case also highlights the critical importance of antiplatelet management, which was shown by the transition from prasugrel to enoxaparin to relieve bleeding risks while preventing thromboembolic events. The sudden increase in creatinine in the postoperative period and the clinical deterioration support the point that early detection and timely intervention are necessary to prevent irreversible renal damage. By presenting this case, we hope to shed light on the challenges and strategies of perioperative care in high-risk patients undergoing urological procedures, thus leading to improved patient outcomes through vigilant and individualized management.
Case Presentation
A 71-year-old male with a history of diabetes, hypertension, dyslipidemia, and ischemic heart disease, treated with PCI and stenting two months prior. The patient presented to the emergency department with a 4-day duration of stabbing flank pain that comes in waves and fluctuates in intensity, nausea, vomiting, confusion, and hematuria.
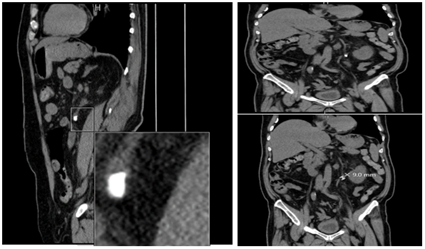
An abdominal un-contrast CT scan revealed obstructive uropathy due to a 9mm left ureteric stone, and laboratory results indicated a creatinine level of 4.3 mg/dL, WBC of 14, 800 cells/mm3. (Figure 1).
Figure 1: Multiple coronal and sagittal cuts of the patient’s abdomen CT scan without IV contrast are shown.
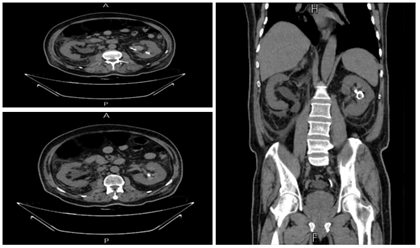
Despite ongoing prasugrel medication, an urgent attempt to place a double-J (DJ) stent failed due to severe obstruction. Consequently, the plan was to switch the patient from prasugrel to enoxaparin for five days before repeating the surgery. During this period, the patient received intravenous antibiotics, and fluids, and maintained of normoglycemia, leading to a progressive decrease in creatinine levels from 3.1 mg/dL to 2.4, 2.1, 1.89, and 1.88 mg/dL, respectively. Two hours after the second DJ stent placement surgery the patient began to complain of worsening bilateral flank pain, nausea, vomiting, hematuria, and creatinine levels increased significantly to 3.7 mg/dL. The unenhanced CT scan ruled out new incidental obstruction, as it showed the migration of the stone to the left kidney (Figure 2).
Figure 2: Multiple coronal and axial cuts of the patient’s abdomen CT scan without IV contrast are shown. Showing both the placed D-j stent and confirming the stone in the left kidney, ruling out any obstruction.
Repeated laboratory tests showed abnormal markers: creatinine of 4.31 mg/dL, BUN of 43 mg/dL, hemoglobin of 11.6 g/dL, and WBC of 14.8 cells/mm³. Within the first 24- hours postoperatively, the patient developed anuria, with laboratory tests of: creatinine at 4.7 mg/dL, BUN at 45 mg/dL, hemoglobin at 10.9 g/dL, and WBC at 15.3 cells/mm³, all suggesting stage 3 AKI. As there is no specific pharmacotherapy for treating AKI, this patient was managed in terms of supporting his kidneys and preventing further damage. We managed the patient by maintaining optimal blood pressure, vital signs, and normoglycemia, as well as we kept monetarizing of serum creatinine, blood urea nitrogen, and electrolytes, giving intravenous antibiotics and fluids to restore dehydration, and carefully balancing fluid intake and output. Moreover, it is important to switch and adjust the dosage of medications to decrease the risk of bleeding and nephrotoxicity. A gradual improvement of kidney function was observed over the following weeks. The patient was referred to do lithotripsy after taking cardiology fitness.
Discussion
Acute kidney injury in this patient appears to be multifactorial. The potential causes for this case include obstructive uropathy from a 9mm left kidney stone, diabetic nephropathy, medication effects, and perioperative hemodynamic changes. Obstructive uropathy, which was obvious by the patient's fluctuating creatinine levels and the initial failed attempt for DJ stent placement, is a contributor. The use of medications such as prasugrel and enoxaparin may have exacerbated the renal impairment. Additionally, the patient’s diabetic status more likely predisposed him to a higher risk of nephropathy, contributing to the AKI.
It is imperative to observe Acute Kidney Injury in patients with diabetes mellitus and multiple comorbid conditions during less invasive procedures like DJ stent placement. Our key insights focused on the importance of early identification and intervention for obstructive uropathy to prevent the progression of AKI.
Reducing AKI risk involves minimizing nephrotoxic drugs in patients with pre-existing renal impairment. Additionally, it is essential to maintain optimal blood pressure, ensure adequate hydration, and closely monitor renal function and electrolytes. However, this case also raises an understanding of the need to involve nephrology, urology, and cardiology since these conditions may be interconnected to affect the overall outcome of AKI in high-risk patients.
In the current case study, we have shown that elderly patients with DM have a greater risk of developing AKI when performing considered safe surgeries such as ureteral stent placement. Interestingly, while acute kidney injury is a well-documented research complication in major abdominal surgeries. On the other hand, AKI is not commonly expected following less invasive procedures such as DJ stent placement.
A comparison with similar cases has shown that the incidence of AKI following bilateral ureteral stent placement during colorectal resection surgery, can be as high as 41.9%. A retrospective analysis at a single community hospital identified that the overall incidence of AKI for non-stented surgeries was 0.8%, compared to 5.8% for both non-lighted and lighted stents. Significant factors influencing AKI incidence included patient age and sex, with higher risks observed in patients over 60 and female patients. Despite these risks, AKI resolved completely in all cases [8].
Learning Points
- Diabetic patients undergoing DJ stent placement are at higher risk of AKI due to pre-existing nephropathy.
- Perioperative management, including fluid balance, antiplatelet therapy adjustments, and nephrotoxic medication review, is essential to prevent complications.
- Early detection and intervention in AKI can lead to reversible kidney injury and better outcomes.
Limitations
During this case we faced some limitations, including usage the non-contrast CT, as contrast reduce renal blood flow in the medulla, induce free oxygen radicals, and induce apoptosis of renal tubular cells [10]. Thus, non-contrast CT is beneficial in avoiding nephrotoxicity, but they have significant limitations in providing a detailed anatomical assessment. Moreover, these findings are from a single patient and cannot be generalized; more research is needed to validate these observations.
Conclusion
The management of postoperative AKI must begin before surgery, with the identification of high-risk patients and optimization of clinical status before and during surgery to prevent the occurrence of AKI [7]. Interestingly, this case highlights the need of further research to validate findings.
Patient Perspective
From the patient's perspective, managing complex health conditions, including diabetes and the need for medications like Plavix to prevent blood clots, added layers of both anxiety and relief. While understanding the necessity of Plavix for cardiovascular protection, the patient expressed concerns about its implications in the context of his AKI episode, as well as its potential role in the healing process post-procedure. This case highlights the patient's experience of balancing treatment benefits with the perceived risks of adverse events.
The patient emphasized gratitude towards the healthcare team for their prompt response and comprehensive care, which he believes contributed to his recovery. Additionally, he hopes that sharing his experience can inform healthcare providers and patients about potential risks associated with similar procedures.
Abbreviations
AKI: Acute Kidney Injury
DM: Diabetes Mellitus
HTN: Hypertension
PCI: Percutaneous Coronary Intervention
DJ stent: Double-J Stent
BUN: Blood Urea Nitrogen
WBC: White Blood Cell
Declarations
Ethics Approval and Consent to Participate
This case report was conducted in accordance with the ethical standards of the institutional and national research committees. Written informed consent for publication was obtained from the patient, and all efforts were made to ensure patient confidentiality.
Consent for Publication
Written informed consent for the publication of this case report and accompanying images was obtained from the patient. This consent complies with ethical standards for the use of individual data in accordance with the journal's editorial policies.
Availability of Data and Materials
The datasets generated during the current study include clinical reports and imaging data related to the patient's case. These datasets are not publicly available to protect patient privacy, but relevant laboratory reports and imaging related to this study will be attached as related files for reference. Interested parties can access these supplementary materials directly with the manuscript.
Competing Interests
The authors declare no competing interests.
Funding
No specific grant or financial support was received for this research from any funding agency in the public, commercial, or not-for-profit sectors.
Authors' Contributions
A.A. (Dr. Ansam Aljaghoub), A.A. (Dr. Anhar Alassali), and A.A.Q. (Dr. Areeb Ahmad Quraish) contributed equally to the conceptualization and design of the case report. A.A. (Dr. Ansam Aljaghoub) collected the clinical data, performed the literature review, and drafted the initial manuscript. A.A. (Dr. Anhar Alassali) provided critical analysis, supervised the development of the manuscript, and contributed to its writing and revision. A.A.Q. (Dr. Areeb Ahmad Quraish) assisted in data collection and provided valuable insights throughout the manuscript preparation. All authors reviewed and approved the final version of the manuscript.
References
- Rahoui M, Ouanes Y, Chaker K, Mrad Dali K, Bibi M, et al. (2022). Life-Threatening Complication Due to Double-J Stent: Renal Subcapsular Hematoma. J Surg Case Rep. 7:rjac329.
Publisher | Google Scholor - Bellomo R, Kellum JA, Ronco C. (2012). Acute Kidney Injury. Lancet. 380(9843):756-766.
Publisher | Google Scholor - Fowler MJ. (2008). Microvascular and Macrovascular Complications of Diabetes. Clin Diabetes. 26(2):77-82.
Publisher | Google Scholor - Venguidesvarane AG, Jasmine A, Varadarajan S, et al. (2020). Prevalence Of Vascular Complications Among Type 2 Diabetic Patients in A Rural Health Center in South India. J Prim Care Community Health. 11:2150132720959962.
Publisher | Google Scholor - KDIGO Acute Kidney Injury Work Group. (2012). KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int Suppl. 2(1):1-138.
Publisher | Google Scholor - Miyaoka R, Monga M. (2009). Ureteral Stent Discomfort: Etiology and Management. Indian J Urol. 25(4):455-460.
Publisher | Google Scholor - Gameiro J, Fonseca JA, Marques F, Lopes JA. (2020). Management of Acute Kidney Injury Following Major Abdominal Surgery: A Contemporary Review. J Clin Med. 9(8):2679.
Publisher | Google Scholor - Moez Rahoui, Yassine Ouanes, Kays Chaker, Kheireddine Mrad Dali, Mokhtar Bibi, et al. (2022). Life-Threatening Complication Due to Double-J Stent: Renal Subcapsular Hematoma, Journal of Surgical Case Reports, 7:rjac329.
Publisher | Google Scholor - Shiyovich A, Skalsky K, Steinmetz T, Ovdat T, Eisen A, et al. (2021). Acute Kidney Injury Following Admission with Acute Coronary Syndrome: The Role of Diabetes Mellitus. J Clin Med. 10(21):4931.
Publisher | Google Scholor - Vandenberghe W, Hoste E. (2019). Contrast-Associated Acute Kidney Injury: Does It Really Exist, And If So, What to Do About It? F1000Res. 8:F1000 Faculty Rev-753.
Publisher | Google Scholor - Aljuhayman A, Balaraj F, Ghazwani Y, Hamri SB. (2020). Subcapsular Double-J Stent Following Ureteroscopy: Unique Complication. J Surg Case Rep. 10:rjaa404.
Publisher | Google Scholor - Chao CT, Wang J, Wu HY, Huang JW, Chien KL. (2018). Age Modifies the Risk Factor Profiles for Acute Kidney Injury Among Recently Diagnosed Type 2 Diabetic Patients: A Population-Based Study. Geroscience. 40(2):201-217.
Publisher | Google Scholor