Research Article
Abdominal Tuberculosis: Infectious Disease of The Whole Society
1Department of Chemistry Sri J.N.M.PG College Lucknow UP India.
2Department of Chemistry Dayanand Girls PG Kanpur UP India.
*Corresponding Author: D.K. Awasthi, Department of Chemistry, Sri J.N.M.PG College, Lucknow UP, India.
Citation: D.K. Awasthi, Dixit A. (2023). Abdominal Tuberculosis: Infectious Disease of The Whole Society. Clinical and Laboratory Research, BioRes Scientia Publishers. 1(1):1-5. DOI: 10.59657/clr.brs.23.001
Copyright: © 2023 D.K. Awasthi, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: May 10, 2023 | Accepted: May 24, 2023 | Published: May 31, 2023
Abstract
Tuberculosis is an infectious disease of the whole society today, capable of spreading and endangering the lives of patients. In particular, intestinal tuberculosis is a very common type of tuberculosis in developing countries, with few typical clinical symptoms and some dangerous complications caused by intestinal. tuberculosis. Abdominal Tuberculosis (TB) affects the gastrointestinal system of the body and impacts the peritoneum, the abdominal lymph nodes and sometimes the intestine itself or rarely, in some cases, abdominal TB can affect the kidney, liver and pancreas. Abdominal Tuberculosis can be seen in both adults and children and can be dangerous for people as it can lead to complications such as acute obstruction of bowel or rupture of the bowel which in some cases also may be life-threatening for people.
Keywords: tuberculosis; digestive system; infection
Introduction
Intestinal tuberculosis is a tuberculosis disease located in the human digestive system, often easily confused with some other digestive diseases. Intestinal tuberculosis is common in patients between the ages of 30 and 55 years old, often accompanied by other TB lesions such as pulmonary tuberculosis. Intestinal tuberculosis can be primary or secondary due to infection with TB bacteria from other organs in the body. For primary intestinal tuberculosis, the cause was found to be caused by bovine tuberculosis bacteria infecting the body through food mediated by cow's milk, which is very rare in clinical practice. In contrast, secondary intestinal tuberculosis is more common and is caused by the patient's contact or ingestion of sputum containing the pathogenic TB bacteria. Secondary intestinal TB can be acquired after a patient has pulmonary, esophageal, peritoneal, or oropharyngeal TB. TB bacteria enter the intestine through the gastrointestinal tract, colonize the intestine and then continue to other structures such as blood or bile. Intestinal tuberculosis bacteria can be human tuberculosis bacteria, animal tuberculosis bacteria such as buffaloes, cows or pigs. Tuberculosis bacteria can enter the small intestine and ileum because they are likely to be unaffected by the gastric juices due to the protective fatty coating, in addition, TB bacteria can also invade some organs. other digestive system such as jejunum and duodenum thanks to this feature. If there is an excess of lymphatic tissue and there are few digestive bacteria as well as stagnation in the ileum, favorable conditions for the formation of ileocecal tuberculosis are created.
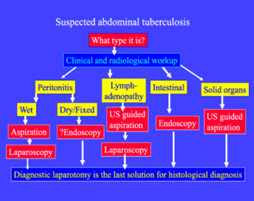
Figure-1
“The main cause of Abdominal Tuberculosis can be the ingestion of germs of tuberculosis. Tuberculosis from the lungs can spread to the abdominal area leading to Abdominal Tuberculosis. It can give a tough time to one’s overall well-being. It will interfere with one’s ability to do the daily chores with ease.”
There can be symptoms such as unintentional loss of weight and persistent abdominal pain along with abdominal distention as well, constipation or some time loose motion with or without bleeding which do not respond to routine medication.” In addition, tuberculosis bacteria from the blood to the intestines and cause diseases, such as millet tuberculosis, are also the cause of intestinal tuberculosis. Another remarkable point is that when TB bacilli are in the dormant stage, they can completely be activated to cause disease if the patient's immune system is weakened and is not resistant to these bacteria.
Fever, unexplained weight loss, body weakness, or night sweats Nausea Abdominal pain, can be localized or pain throughout the abdomen, especially the right iliac fossa. There may be abdominal cramps, abdominal cramps... Diarrhea for a long time Passing may have blood in the stool Constipation Risk factors that increase the likelihood of intestinal tuberculosis include:
Infection of GIT by mycobacteria can occur in five ways:
- Sputum ingestion by a patient with active pulmonary disease from Mycobacterium tuberculosis.
- Hematogenous spread from a distant focus.
- Lymphatic spread through infected nodes.
- Direct extension from a contiguous site.
- Ingestion of milk products infected with Mycobacterium bovis – particularly seen with consumption of raw milk.
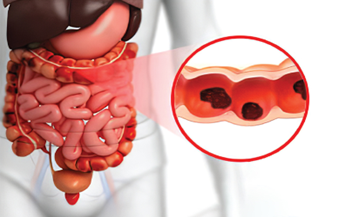
Figure 2: Abdominal T.B.
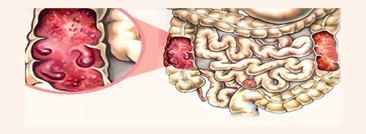
Figure-3: Gastrointestinal T.B.
Esophageal TB
Esophageal involvement in TB occurs rarely. It has been seen to occur due to spread from adjacent tissues. It usually involves the middle one-third of the esophagus, at the level of the carina
It may present with dysphagia and odynophagia.
Gastric and Gastroduodenal TB
Due to the protective fatty acid capsule of mycobacteria (as described earlier), proximal GIT lesions were thought to be rare. Additional factors that were thought to prevent TB in the stomach and duodenum were a high acid environment, rapid transit time, and a relative absence of lymphoid tissue. However, they have been reported in the stomach and duodenum. It is reported to occur secondary to pulmonary TB. Gastrointestinal (GI) tuberculosis in this anatomic location may lead to gastric outlet obstruction and surgical obstructive jaundice
TB of the Small and Large Intestine
Four major forms have been reported:Ulcerative – the most common form. Usually presents with superficial transverse ulcers. It is more likely to be seen in the small intestine.
- Hypertrophic – occurs as a hyperplastic reaction around the ulcer, producing an inflammatory mass. It is more likely to be seen in the cecum.
- Ulcero-hypertrophic – a combination of ulcerative and hypertrophic forms may occur.
- Fibrous stricturing – may lead to fibrosis and stricture formation, resulting in intestinal obstruction.
Rectal and Anal TB
TB involving the rectal and anal areas may present as multiple fistulae (mimicking Crohn disease), a non-healing lesion after recent anal surgery or a circumferential mass resembling rectal prolapse.
Solid Organ TB:
Solid organs may be involved by hematogenous dissemination or direct intra-abdominal spread.
Peritoneal TB
Peritoneal TB usually occurs with other forms of abdominal TB, with peritoneal involvement occurring after the rupture of necrotic lymph nodes. Lymph nodes in the small bowel mesentery and the retroperitoneum are commonly involved, and these may caseate and calcify. Ascites is the most frequent manifestation.
Peritoneal Involvement
TB peritonitis exists in 5 main forms:
- Ascitic
- Loculated (encysted)
- Plastic (fibrous)
- Purulent
- Nodular
Ischemia caused by vascular thrombosis may be responsible for tissue breakdown when there is the involvement of mesenteric vasculature by granulomatous inflammation was commonly associated with the ulcerative type with perforation. This suggests that ischemia secondary to vascular thrombosis is responsible for tissue breakdown. This implies that vasculitis plays an important role in the natural history of abdominal tuberculosis. Patients with gastrointestinal tuberculosis commonly present with the following complaints: Abdominal pain.
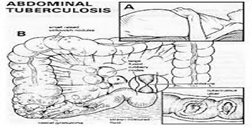
Figure 4
- Anorexia
- Fever
- Change in bowel habits – diarrhea more common than constipation
- Nausea and vomiting
- Melena
On examination, they are commonly found to have the following signs:
- Weight loss
- Pallor and anemia
- Rectal bleeding
- Abdominal distension and ascites
- Hepatomegaly
- Splenomegaly
- Lymphadenopathy
- Abdominal mass
A family history of TB may not be evident in all patients. Thus, GI TB must be considered even in the absence of family history. Similarly, only a few patients may have concomitant pulmonary TB or a past medical history of TB.
General Laboratory Testing
Patients with gastrointestinal tuberculosis are noted to have lower hemoglobin levels, lower serum albumin, and high C-reactive protein (CRP) levels. CRP, erythrocytes sedimentation rate (ESR), and fecal calprotectin may also be useful in follow-up as a surrogate marker for healing while on antituberculosis treatment (ATT).
Conclusion
Tuberculosis (TB) is a life-threatening disease which can virtually affect any part of the gastrointestinal tract. According to World Health Organization report 2015, there was an estimated annual incidence of 9 million of TB globally. India has the world’s largest tuberculosis cases which is around 26% of the world TB cases, followed by China and South Africa the primary site of TB is usually lung, from where it disseminates to other parts of the body. TB of the gastrointestinal tract is the sixth most frequent form of extra-pulmonary site, after lymphatic, genitourinary, bone and joint, miliary and meningeal tuberculosis. The abdominal TB is usually diagnosed late due to its rare presentation and the diagnosis requires a high index of suspicion. It affects both genders equally and the most common age of presentation is 10-25 yrs. The abdominal TB usually occurs in four forms: tuberculous lymphadenopathy, peritoneal tuberculosis, gastrointestinal (GI) tuberculosis and visceral tuberculosis. Computed tomography (CT) appears to be the imaging modality of choice in the detection and assessment of abdominal TB.
References
- Sheer TA, Coyle WJ. (2003). Gastrointestinal tuberculosis. Curr Gastroenterol Rep., 5(4):273-278.
Publisher | Google Scholor - Farer LS, Lowell AM, Meador MP. (1979). Extrapulmonary tuberculosis in the United States. Am J Epidemiol, 109(2):205-217.
Publisher | Google Scholor - Horvath KD, Whelan RL. (1998). Intestinal tuberculosis: return of an old disease. Am J Gastroenterol., 93(5):692-696.
Publisher | Google Scholor - Rathi P, Gambhire P. (2016). Abdominal Tuberculosis. J Assoc Physicians India, 64(2):38-47.
Publisher | Google Scholor - de la Rua-Domenech R. (2006). Human Mycobacterium bovis infection in the United Kingdom: Incidence, risks, control measures and review of the zoonotic aspects of bovine tuberculosis. Tuberculosis (Edinb), 86(2):77-109.
Publisher | Google Scholor - Al-Bahrani ZR, Al-Saleem T. (1982). Intestinal tuberculosis in Iraq: a study of 50 cases. Int Surg. 67(4):483-485.
Publisher | Google Scholor - Palmer KR, Patil DH, Basran GS, Riordan JF, Silk DB. (1985). Abdominal tuberculosis in urban Britain--a common disease. Gut, (12):1296-1305.
Publisher | Google Scholor - Kasulke RJ, Anderson WJ, Gupta SK, Gliedman ML. (1981). Primary tuberculous enterocolitis. Report of three cases and review of the literature. Arch Surg., 116(1):110-113.
Publisher | Google Scholor - Tabrisky J, Lindstrom RR, Peters R, Lachman RS. (1975). Tuberculous enteritis. Review of a protean disease. Am J Gastroenterol. 1975 Jan;63(1):49-57.
Publisher | Google Scholor - Zhang XF, Lv Y, Xue WJ, Wang B, Liu C, Tian PX, Yu L, Chen XY, Liu XM. (2008). Mycobacterium tuberculosis infection in solid organ transplant recipients: experience from a single center in China. Transplant Proc. 2008 Jun;40(5):1382-1385.
Publisher | Google Scholor - Zedtwitz-Liebenstein K, Podesser B, Peck-Radosavljevic M, Graninger W. Intestinal tuberculosis presenting as fever of unknown origin in a heart transplant patient. Infection. 1999;27(4-5):289-290.
Publisher | Google Scholor - Shad S, Rai AA, Soomro GB, Luck NH. (2018). Tuberculous Paraspinal Abscess Invading Esophagus: A Rare Cause of Dysphagia. J Coll Physicians Surg Pak., 28(7):566-567.
Publisher | Google Scholor - Dahale AS, Kumar A, Srivastava S, Varakanahalli S, Sachdeva S, Puri AS. (2018). Esophageal tuberculosis: Uncommon of common. JGH Open, 2(2):34-38.
Publisher | Google Scholor - Balikian JP, Yenikomshian SM, Jidejian YD. (1967). Tuberculosis of the pyloro-duodenal area. Report of four cases. Am J Roentgenol Radium Ther Nucl Med, 101(2):414-420.
Publisher | Google Scholor - Arabi NA, Musaad AM, Ahmed EE, Ibnouf MM, Abdelaziz MS. (205). Primary gastric tuberculosis presenting as gastric outlet obstruction: a case report and review of the literature. J Med Case Rep, 18(9):265.
Publisher | Google Scholor - Rodriguez-Takeuchi SY, Renjifo ME, Medina FJ. (2019). Extrapulmonary Tuberculosis: Pathophysiology and Imaging Findings. Radiographics, 39(7):2023-2037.
Publisher | Google Scholor - Muneef MA, Memish Z, Mahmoud SA, Sadoon SA, Bannatyne R, et al. (2001). Tuberculosis in the belly: a review of forty-six cases involving the gastrointestinal tract and peritoneum. Scand J Gastroenterol, 36(5):528-532.
Publisher | Google Scholor - Sato S, Yao K, Yao T, Schlemper RJ, Matsui T. et al. (2004). Colonoscopy in the diagnosis of intestinal tuberculosis in asymptomatic patients. Gastrointest Endosc., 59(3):362-368.
Publisher | Google Scholor - Arend SM, Leyten EM, Franken WP, Huisman EM, van Dissel JT. (2007). A patient with de novo tuberculosis during anti-tumor necrosis factor-alpha therapy illustrating diagnostic pitfalls and paradoxical response to treatment. Clin Infect Dis, 45(11):1470-1475
Publisher | Google Scholor - Lin PY, Wang JY, Hsueh PR, Lee LN, Hsiao CH, Yu CJ, Yang PC. (2009). Lower gastrointestinal tract tuberculosis: an important but neglected disease. Int J Colorectal Dis., 24(10):1175-1180.
Publisher | Google Scholor